About Basal and Squamous Cell Skin Cancer
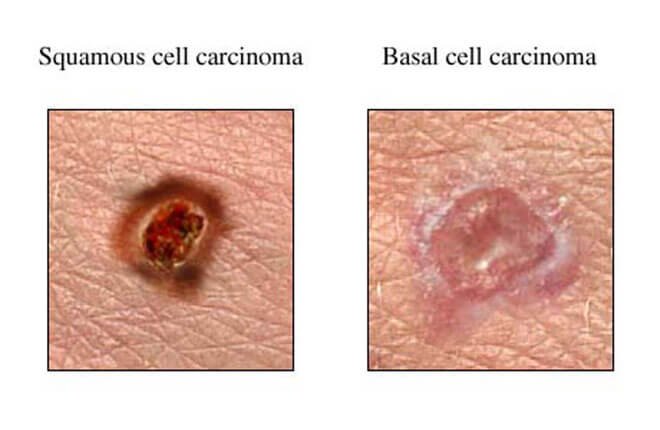
Basal cell carcinoma usually affects the head, neck, back, chest, or shoulders. The nose is the most common site. Signs of basal cell carcinoma can include skin changes such as a:
- Firm, pearly bump with tiny bloodvessels that look spidery (telangiectasias).
- Red, tender, flat spot that bleeds easily.
- Small, fleshy bump with a smooth, pearly appearance, often with a depressed center.
- Smooth, shiny bump that may look like a mole or cyst.
- Patch of skin, especially on the face, that looks like a scar and is firm to the touch.
- Bump that itches, bleeds, crusts over, and then repeats the cycle and has not healed in 3 weeks.
- Change in the size, shape, or color of a mole or a skin growth.
Squamous cell carcinoma usually affects the face, head, or neck. Signs of squamous cell carcinoma include any:
- Persistent, firm, red bump on sun-exposed skin.
- Patch of skin that feels scaly, bleeds, or develops a crust. The patch may get bigger over a period of months and form a sore.
- Skin growth that looks like a wart.
- Sore that does not heal or an area of thickened skin on the lower lip, especially if you smoke or use chewing tobaccoor your lips are often exposed to the sun and wind.
Types of skin cells
There are 3 main types of cells in the top layer of the skin (called the epidermis):
- Squamous cells: These are flat cells in the outer part of the epidermis that are constantly shed as new ones form.
- Basal cells: These cells are in the lower part of the epidermis, called the basal cell layer. These cells constantly divide to form new cells to replace the squamous cells that wear off the skin’s surface. As these cells move up in the epidermis, they get flatter, eventually becoming squamous cells.
- Melanocytes: These cells make the brown pigment called melanin, which gives the skin its tan or brown color. Melanin acts as the body’s natural sunscreen, protecting the deeper layers of the skin from some of the harmful effects of the sun. For most people, when skin is exposed to the sun, melanocytes make more of the pigment, causing the skin to tan or darken.
The epidermis is separated from the deeper layers of skin by the basement membrane. When a skin cancer becomes more advanced, it generally grows through this barrier and into the deeper layers.
Types of skin cancer
Basal cell carcinoma
This the most common type of skin cancer. About 8 out of 10 skin cancers are basal cell carcinomas (also called basal cell cancers). When seen under a microscope, the cells in these cancers look like cells in the lowest layer of the epidermis, called the basal cell layer.
These cancers usually develop on sun-exposed areas, especially the head and neck. These cancers tend to grow slowly. It’s very rare for a basal cell cancer to spread to other parts of the body. But if a basal cell cancer is left untreated, it can grow into nearby areas and invade the bone or other tissues beneath the skin.
If not removed completely, basal cell carcinoma can recur (come back) in the same place on the skin. People who have had basal cell skin cancers are also more likely to get new ones in other places.
Squamous cell carcinoma
About 2 out of 10 skin cancers are squamous cell carcinomas (also called squamous cell cancers). The cells in these cancers look like abnormal versions of the squamous cells seen in the outer layers of the skin.
These cancers commonly appear on sun-exposed areas of the body such as the face, ears, neck, lips, and backs of the hands. They can also develop in scars or chronic skin sores elsewhere. They sometimes start in actinic keratoses (described below). Less often, they form in the skin of the genital area.
Squamous cell cancers are more likely to grow into deeper layers of skin and spread to other parts of the body than basal cell cancers, although this is still uncommon.
Keratoacanthomas are dome-shaped tumors that are found on sun-exposed skin. They may start out growing quickly, but their growth usually slows down. Many keratoacanthomas shrink or even go away on their own over time without any treatment. But some continue to grow, and a few may even spread to other parts of the body. Their growth is often hard to predict, so many skin cancer experts consider them a type of squamous cell skin cancer and treat them as such.
Melanoma
These cancers develop from melanocytes, the pigment-making cells of the skin. Melanocytes can also form benign (non-cancerous) growths called moles. Melanomas are much less common than basal and squamous cell cancers, but they are more likely to grow and spread if left untreated. Melanoma and moles are discussed in Melanoma Skin Cancer.
Less common types of skin cancer
Other types of skin cancer are much less common and are treated differently. These include:
- Merkel cell carcinoma
- Kaposi sarcoma
- Cutaneous (skin) lymphoma
- Skin adnexal tumors (tumors that start in hair follicles or skin glands)
- Various types of sarcomas
Together, these types account for less than 1% of all skin cancers.
Pre-cancerous and pre-invasive skin conditions
These conditions may develop into skin cancer or may be very early stages of skin cancer.
Actinic keratosis (solar keratosis)
Actinic keratosis (AK), also known as solar keratosis, is a pre-cancerous skin condition caused by too much exposure to the sun. AKs are usually small (less than 1/4 inch across), rough or scaly spots that may be pink-red or flesh-colored. Usually they start on the face, ears, backs of the hands, and arms of middle-aged or older people with fair skin, although they can occur on other sun-exposed areas. People who have them usually develop more than one.
AKs tend to grow slowly and usually do not cause any symptoms (although some might be itchy or sore). They sometimes go away on their own, but they may come back.
Some AKs may turn into squamous cell skin cancers. Most AKs do not become cancer, but it can be hard sometimes to tell them apart from true skin cancers, so doctors often recommend treating them. If they are not treated, you and your doctor should check them regularly for changes that might be signs of skin cancer.
Squamous cell carcinoma in situ (Bowen disease)
Squamous cell carcinoma in situ, also called Bowen disease, is the earliest form of squamous cell skin cancer. “In situ” means that the cells of these cancers are still only in the epidermis (the upper layer of the skin) and have not invaded into deeper layers.
Bowen disease appears as reddish patches. Compared with AKs, Bowen disease patches tend to be larger (sometimes over ½ inch across), redder, scalier, and sometimes crusted. Like AK, Bowen disease usually doesn’t cause symptoms, although it might be itchy or sore.
Like most other skin cancers (and AKs), these patches most often appear in sun-exposed areas. Bowen disease can also occur in the skin of the anal and genital areas (where it is known as erythroplasia of Queyrat or Bowenoid papulosis). This is often related to sexually transmitted infection with human papilloma viruses (HPVs), the viruses that can also cause genital warts.
Bowen disease can sometimes progress to an invasive squamous cell skin cancer, so doctors usually recommend treating it. People who have these are also at higher risk for other skin cancers, so close follow-up with a doctor is important.
Benign skin tumors
Most skin tumors are benign (not cancerous) and rarely if ever turn into cancers. There are many kinds of benign skin tumors, including:
- Most types of moles (see Melanoma Skin Cancerfor more about moles)
- Seborrheic keratoses: tan, brown, or black raised spots with a waxy texture or occasionally a slightly rough and crumbly surface when they are on the legs (also known as stucco keratosis)
- Hemangiomas: benign blood vessel growths, often called strawberry spots
- Lipomas: soft tumors made up of fat cells
- Warts: rough-surfaced growths caused by some types of human papilloma virus (HPV)
Risk Factors
A risk factor is anything that affects your chance of getting a disease such as cancer. Different cancers have different risk factors. Some risk factors, like smoking and excess sun exposure, can be changed. Others, like your age or family history, can’t be changed.
Having a risk factor, or even many risk factors, does not mean that you will get skin cancer. Many people with risk factors for skin cancer, never get it. Others with this disease may have few or no known risk factors.
Still, it’s important to know about the risk factors for skin cancer because there may be things you can do that could lower your risk of getting it. If you are at higher risk because of certain factors, there are also things you can do that might help find it early, when it’s likely to be easier to treat.
Several risk factors make a person more likely to get basal cell or squamous cell skin cancer. (These factors don’t necessarily apply to some other forms of skin cancer, such as Kaposi sarcoma and skin lymphoma.)
Ultraviolet (UV) light exposure
Exposure to ultraviolet (UV) rays is thought to be the major risk factor for most skin cancers. Sunlight is the main source of UV rays. Tanning beds are another source of UV rays.
While UV rays make up only a very small portion of the sun’s rays, they are the main cause of the damaging effects of the sun on the skin. UV rays damage the DNA of skin cells. Skin cancers begin when this damage affects the DNA of genes that control skin cell growth. To learn more about the effects of UV rays on the skin and what you can do to protect yourself and your loved ones, see Skin Cancer Prevention and Early Detection.
Having light-colored skin
Whites have a much higher risk of skin cancer than African Americans or Hispanics. This is because the skin pigment melanin has a protective effect in people with darker skin. Whites with fair (light-colored) skin that freckles or burns easily are at especially high risk.
Albinism is an inherited lack of protective skin pigment. People with this condition may have pink-white skin and white hair. They have a high risk of getting sunburns and skin cancer, so they need to be careful to protect their skin.
Being older
The risk of getting basal and squamous cell skin cancers rises as people get older. This is probably because of the buildup of sun exposure over time. These cancers are becoming more common in younger people as well, probably because they are spending more time in the sun with their skin exposed.
Being male
Men are more likely than women to have basal and squamous cell cancers of the skin. This is thought to be due mainly to getting more sun exposure.
Exposure to certain chemicals
Being exposed to large amounts of arsenic increases the risk of developing skin cancer. Arsenic is an element found naturally in well water in some areas. It’s also used in making some pesticides and in some other industries.
Workers exposed to coal tar, paraffin, and certain types of oil may also have an increased risk of skin cancer.
Radiation exposure
People who have had radiation treatment have a higher risk of developing skin cancer in the area that received the treatment. This is particularly a concern in children who have had radiation treatment for cancer.
Previous skin cancer
People who have had a basal or squamous cell cancer have a much higher chance of developing another one.
Long-term or severe skin inflammation or injury
Scars from severe burns, areas of skin over serious bone infections, and skin damaged by some severe inflammatory skin diseases are more likely to develop skin cancers, although this risk is generally small.
Psoriasis treatment
Psoralens and ultraviolet light (PUVA) treatments given to some patients with psoriasis (a long-lasting inflammatory skin disease) can increase the risk of developing squamous cell skin cancer and probably other skin cancers.
Xeroderma pigmentosum (XP)
This very rare inherited condition reduces the ability of skin cells to repair DNA damage caused by sun exposure. People with this disorder often develop many skin cancers, starting in childhood.
Basal cell nevus syndrome (also known as nevoid basal cell carcinoma syndrome or Gorlin syndrome)
In this rare congenital (present at birth) condition, people develop many basal cell cancers over their lifetime. People with this syndrome may also have abnormalities of the jaw (and other bones), eyes, and nervous tissue.
Most of the time this condition is inherited from a parent. In families with this syndrome, those affected often start to develop basal cell cancers as children or teens. Exposure to UV rays can increase the number of tumors these people get.
Weakened immune system
The immune system helps the body fight cancers of the skin and other organs. People with weakened immune systems (from certain diseases or medical treatments) are more likely to develop many types of skin cancer, including squamous cell cancer, melanoma, and less common types such as Kaposi sarcoma and Merkel cell carcinoma.
For example, people who get organ transplants are usually given medicines that weaken their immune system to help prevent their body from rejecting the new organ. This increases their risk of developing skin cancer. Skin cancers in people with weakened immune systems tend to grow faster and are more likely to be fatal.
Treatment with large doses of corticosteroid drugs can also weaken the immune system. This may also increase a person’s risk of skin cancer.
People infected with HIV, the virus that causes AIDS, often have weakened immune systems and also are at increased risk for basal and squamous cell cancers.
Human papilloma virus (HPV) infection
Human papilloma viruses (HPVs) are a group of more than 150 viruses, many of which can cause papillomas, or warts. The warts that people commonly get on their hands and feet are not related to any form of cancer. But some HPV types, especially those that affect the genital and anal areas and the skin around the fingernails, seem to be related to skin cancers in these areas.
Smoking
People who smoke are more likely to develop squamous cell skin cancer, especially on the lips. Smoking is not a known risk factor for basal cell cancer.
Causes
While many risk factors for basal and squamous cell skin cancers have been found, it’s not always clear exactly how these factors might cause cancer.
Most basal cell and squamous cell skin cancers are caused by repeated and unprotected skin exposure to ultraviolet (UV) rays from sunlight, as well as from man-made sources such as tanning beds.
UV rays can damage the DNA inside skin cells. DNA is the chemical in each of our cells that makes up our genes, which control how our cells function. We usually look like our parents because they are the source of our DNA. But DNA affects more than just how we look.
Some genes help control when our cells grow, divide into new cells, and die:
- Genes that help cells grow, divide, and stay alive are called oncogenes.
- Genes that keep cell growth in check by slowing down cell division or causing cells to die at the right time are called tumor suppressor genes.
Cancers can be caused by DNA changes that turn on oncogenes or turn off tumor suppressor genes. Changes in several different genes are usually needed for a cell to become cancer.
Researchers don’t yet know all of the DNA changes that result in skin cancer, but they have found that in many skin cancers the cells have changes in tumor suppressor genes. The gene most often altered in squamous cell cancers is called TP53. This tumor suppressor gene normally causes cells with damaged DNA to die. When TP53 is altered, these abnormal cells may live longer and perhaps go on to become cancerous.
A gene often mutated in basal cell cancers is the PTCH1 gene, which is part of the “hedgehog” signaling pathway inside cells. PTCH1 is a tumor suppressor gene that normally helps keep cell growth in check, so changes in this gene can allow cells to grow out of control. People who have basal cell nevus syndrome (Gorlin syndrome), which is often inherited from a parent and results in getting many basal cell cancers, have an altered PTCH1 gene in all the cells of their body.
These are not the only gene changes that play a role in the development of skin cancer. There are likely to be many others as well.
People with xeroderma pigmentosum (XP) have a high risk for skin cancer. XP is a rare, inherited condition resulting from a defect in an enzyme that repairs DNA damage. Because people with XP are less able to repair DNA damage caused by sunlight, they often develop many cancers on sun-exposed areas of their skin.
The link between squamous cell skin cancer and infection with some types of the human papilloma virus (HPV) also involves DNA and genes. These viruses have genes that affect growth-regulating proteins of infected skin cells. This can cause skin cells to grow too much and to not die when they’re supposed to.
Scientists are studying other links between DNA changes and skin cancer. A better understanding of how damaged DNA leads to skin cancer might be used to design treatments to overcome or repair that damage.
Can Basal and Squamous Cell Skin Cancers Be Found Early?
Basal cell and squamous cell skin cancers can often be found early, when they are likely to be easier to treat.
Skin self-exam
Although the American Cancer Society does not have guidelines for the early detection of skin cancer, knowing your own skin is important to finding skin cancer early. Learn the patterns of moles, blemishes, freckles, and other marks on your skin so that you’ll notice any changes.
Many doctors recommend checking your skin, preferably once a month. Skin self-exams are best done in a well-lit room in front of a full-length mirror. Use a hand-held mirror for areas that are hard to see, such as the backs of your thighs. All areas should be examined, including your palms and soles, scalp, ears, nails, and your back. Friends and family members can also help you with these exams, especially for those hard-to-see areas, such as your scalp and back.
Be sure to show your doctor any areas that concern you and ask your doctor to look at areas that may be hard for you to see.
Any spots on the skin that are new or changing in size, shape, or color should be seen by a doctor promptly. Any unusual sore, lump, blemish, marking, or change in the way an area of the skin looks or feels may be a sign of skin cancer or a warning that it might occur. The area might become red, swollen, scaly, crusty or begin oozing or bleeding. It may feel itchy, tender, or painful.
Basal cell and squamous cell skin cancers can look like a variety of marks on the skin. The key warning signs are a new growth, a spot or bump that’s getting larger over time, or a sore that doesn’t heal within a few weeks. (See Signs and Symptoms of Basal and Squamous Cell Skin Cancer for a more detailed description of what to look for.)
Exam by a health care professional
Some doctors and other health care professionals do skin exams as part of routine health check-ups.
Having regular skin exams is especially important for people who are at high risk of skin cancer, such as people with reduced immunity (for example, those who have had an organ transplant) or people with conditions such as basal cell nevus syndrome (Gorlin syndrome) or xeroderma pigmentosum (XP). Talk to your doctor about how often you should have your skin examined.
Prevention and Early Detection
Skin cancer is the most common cancer in the United States. In fact, more skin cancers are diagnosed in the US each year than all other cancers combined. The number of skin cancer cases has been going up over the past few decades.
Most skin cancers are caused by too much exposure to ultraviolet (UV) rays. Most of this exposure comes from the sun, but some may come from man-made sources, such as indoor tanning beds and sun lamps. The good news is that you can do a lot to protect yourself and your family from UV rays, as well as to catch skin cancer early so that it can be treated effectively.
You don’t need x-rays or blood tests to find skin cancer early – just your eyes and a mirror. If you have skin cancer, finding it early is the best way to make sure it can be treated with success.
Signs and Symptoms
Basal cell carcinomas
Basal cell cancers usually develop on areas exposed to the sun, especially the face, head, and neck, but they can occur anywhere on the body.
These cancers can appear as:
- Flat, firm, pale or yellow areas, similar to a scar
- Raised reddish patches that might be itchy
- Small, pink or red, translucent, shiny, pearly bumps, which might have blue, brown, or black areas
- Pink growths with raised edges and a lower area in their center, which might contain abnormal blood vessels spreading out like the spokes of a wheel
- Open sores (which may have oozing or crusted areas) that don’t heal, or that heal and then come back
Basal cell cancers are often fragile and might bleed after shaving or after a minor injury. Sometimes people go to the doctor because they have a sore or a cut from shaving that just won’t heal, which turns out to be a basal cell cancer. A simple rule of thumb is that most shaving cuts heal within a week or so.
Squamous cell carcinomas
Squamous cell cancers tend to occur on sun-exposed areas of the body such as the face, ear, neck, lip, and back of the hands. Less often, they form in the skin of the genital area. They can also develop in scars or skin sores elsewhere.
These cancers can appear as:
- Rough or scaly red patches, which might crust or bleed
- Raised growths or lumps, sometimes with a lower area in the center
- Open sores (which may have oozing or crusted areas) that don’t heal, or that heal and then come back
- Wart-like growths
Both basal and squamous cell skin cancers can also develop as a flat area showing only slight changes from normal skin. To see some examples of basal and squamous cell cancers, visit our Skin Cancer Image Gallery.
These and other types of skin cancers can also look different from the descriptions above. This is why it’s important to have any new or changing skin growths, sores that don’t heal, or other areas that concern you checked by your doctor.
Tests for Basal and Squamous Cell Skin Cancers
Most skin cancers are brought to a doctor’s attention because of signs or symptoms a person is having.
If you have an abnormal area that might be skin cancer, your doctor will examine it and might do tests to find out if it is cancer or some other skin condition. If there is a chance the skin cancer has spread to other areas of the body, other tests might be done as well.
Medical history and physical exam
Usually the first step is for your doctor to ask about your symptoms, such as when the mark first appeared on the skin, if it has changed in size or appearance, and if it has been painful, itchy, or bleeding. You might also be asked about past exposures to causes of skin cancer (including sunburns and tanning practices) and if you or anyone in your family has had skin cancer.
During the physical exam, the doctor will note the size, shape, color, and texture of the area(s) in question, and whether it is bleeding, oozing, or crusting. The rest of your body may be checked for moles and other spots that could be related to skin cancer.
The doctor may also feel the nearby lymph nodes, which are bean-sized collections of immune system cells under the skin in certain areas. Some skin cancers can spread to lymph nodes. When this happens, the lymph nodes might be felt as lumps under the skin.
If you are being seen by your primary doctor and skin cancer is suspected, you may be referred to a dermatologist (a doctor who specializes in skin diseases), who will look at the area more closely.
Along with a standard physical exam, some dermatologists use a technique called dermatoscopy (also known as dermoscopy, epiluminescence microscopy [ELM] or surfacemicroscopy) to see spots on the skin more clearly. The doctor uses a dermatoscope, which is a special magnifying lens and light source held near the skin. Sometimes a thin layer of alcohol or oil is used with this instrument. The doctor may take a digital photo of the spot.
When used by an experienced dermatologist, this test can improve the accuracy of finding skin cancers early. It can also often help reassure you if a spot on the skin is probably benign (non-cancerous) without the need for a biopsy.
Skin biopsy
If the doctor thinks that a suspicious area might be skin cancer, the area (or part of it) will be removed and sent to a lab to be looked at under a microscope. This is called a skin biopsy. If the biopsy removes the entire tumor, it’s often enough to cure basal and squamous cell skin cancers without further treatment.
There are different types of skin biopsies. The doctor will choose one based on the suspected type of skin cancer, where it is on your body, its size, and other factors. Any biopsy will probably leave at least a small scar. Different methods can result in different scars, so if this is a concern, ask your doctor about possible scarring before the biopsy is done.
Skin biopsies are done using a local anesthetic (numbing medicine), which is injected into the area with a very small needle. You will probably feel a small prick and a little stinging as the medicine is injected, but you should not feel any pain during the biopsy.
Shave (tangential) biopsy
For a shave biopsy, the doctor shaves off the top layers of the skin with a small surgical blade. Bleeding from the biopsy site is then stopped by applying an ointment or a chemical that stops bleeding, or by using a small electrical current to cauterize the wound.
Punch biopsy
For a punch biopsy, the doctor uses a tool that looks like a tiny round cookie cutter to remove a deeper sample of skin. The doctor rotates the punch biopsy tool on the skin until it cuts through all the layers of the skin. The sample is removed and the edges of the biopsy site are often stitched together.
Incisional and excisional biopsies
To examine a tumor that may have grown into deeper layers of the skin, the doctor may use an incisional or excisional biopsy.
- An incisional biopsy removes only a portion of the tumor.
- An excisional biopsy removes the entire tumor.
For these types of biopsies, a surgical knife is used to cut through the full thickness of skin. A wedge or sliver of skin is removed for examination, and the edges of the wound are usually stitched together.
Examining the biopsy samples
All skin biopsy samples are sent to a lab, where they are looked at with a microscope by a doctor called a pathologist. Often, the samples are sent to a dermatopathologist, a doctor who has special training in looking at skin samples.
Lymph node biopsy
It’s rare for basal or squamous cell cancer to spread beyond the skin, but if it does it usually goes first to nearby lymph nodes, which are bean-sized collections of immune cells. If your doctor feels lymph nodes under the skin near the tumor that are too large or too firm, a lymph node biopsy may be done to find out if cancer has spread to them.
Fine needle aspiration biopsy
For a fine needle aspiration (FNA) biopsy, the doctor uses a syringe with a thin, hollow needle to remove very small fragments of the lymph node. The needle is smaller than the needle used for a blood test. A local anesthetic is sometimes used to numb the area first. This test rarely causes much discomfort and does not leave a scar.
FNA biopsies are not as invasive as some other types of biopsies, but they may not always provide a large enough sample to find cancer cells.
Surgical (excisional) lymph node biopsy
If an FNA does not find cancer in a lymph node but the doctor still suspects the cancer has spread there, the lymph node may be removed by surgery and examined. If the lymph node is just under the skin, this can often be done in a doctor’s office or outpatient surgical center using local anesthesia. This will leave a small scar.
Living as a Basal or Squamous Cell Skin Cancer Survivor
For most people with basal or squamous cell skin cancers, treatment will remove or destroy the cancer. Completing treatment can be both stressful and exciting. You may be relieved to finish treatment, but find it hard not to worry about cancer growing or coming back. (When cancer comes back after treatment, it is called recurrent cancer or a recurrence.) This is very common if you’ve had cancer.
For a small number of people with more advanced skin cancers, the cancer may never go away completely. These people may get regular treatment with radiation therapy, chemotherapy, or other treatments to help keep the cancer in check for as long as possible. Learning to live with cancer that does not go away can be difficult and very stressful.
For More Information Visit Us Our Website: https://www.healthinfi.com
2 500
No Comments