What Is Emphysema?
Emphysema is a disease of the lungs that usually develops after many years of smoking. Along with asthma and chronic bronchitis, emphysema belongs to a group of lung diseases known as a chronic obstructive pulmonary disease (COPD).
Emphysema is a lung condition that causes shortness of breath. In people with emphysema, the air sacs in the lungs (alveoli) are damaged. Over time, the inner walls of the air sacs weaken and rupture creating larger air spaces instead of many small ones.
This reduces the surface area of the lungs and, in turn, the amount of oxygen that reaches your bloodstream. When you exhale, the damaged alveoli don’t work properly and old air becomes trapped, leaving no room for fresh, oxygen-rich air to enter.
Emphysema is a disease of the lungs that usually develops after many years of smoking. Both chronic bronchitis and emphysema belong to a group of lung diseases known as a chronic obstructive pulmonary disease (COPD). Once it develops, emphysema can’t be reversed. This is why not smoking or stopping smoking is very important.
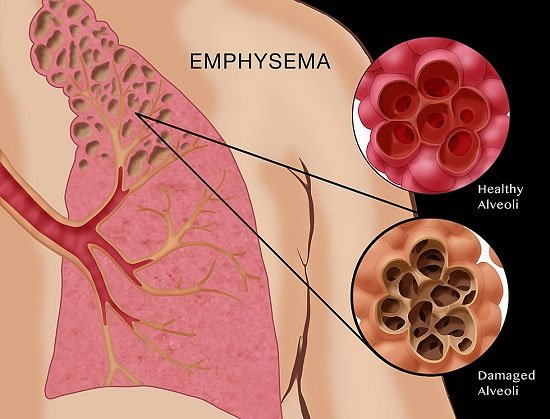
Emphysema is a condition that involves damage to the walls of the air sacs (alveoli) of the lung. Alveoli are small, thin-walled, very fragile air sacs located in clusters at the end of the bronchial tubes deep inside the lungs.
There are about 300 million alveoli in normal lungs. As you breathe in air, the alveoli stretch, drawing oxygen in and transporting it to the blood. When you exhale, the alveoli shrink, forcing carbon dioxide out of the body.
When emphysema develops, the alveoli and lung tissue are destroyed. With this damage, the alveoli cannot support the bronchial tubes. The tubes collapse and cause an “obstruction” (a blockage), which traps air inside the lungs.
Too much air trapped in the lungs can give some patients a barrel-chested appearance. Also, because there are fewer alveoli, less oxygen will be able to move into the bloodstream.
Most people with emphysema also have chronic bronchitis. Chronic bronchitis is inflammation of the tubes that carry air to your lungs (bronchial tubes), which leads to a persistent cough.
Emphysema and chronic bronchitis are two conditions that make up chronic obstructive pulmonary disease (COPD). Smoking is the leading cause of COPD. Treatment may slow the progression of COPD, but it can’t reverse the damage.
In the United States (U.S.), 3.5 million people, or 1.5 percent of the population, received a diagnosis of emphysema in 2016. The number of deaths involving emphysema was 7,455, or 2.3 people in every 100,000.
Who gets emphysema?
Over 3 million people in the United States have been diagnosed with emphysema. Over 11 million Americans have COPD. Emphysema is most common in men between the ages of 50 and 70.
How Does It Happen?
You get emphysema when the linings of the tiny air sacs in your lungs become damaged beyond repair. Over time, your lung damage gets worse. Here’s what happens:
- The fragile tissues between air sacs are destroyed and air pockets form in the lungs.
- Air gets trapped in these pouches of damaged tissue.
- The lungs slowly get larger, and you find it harder to breathe.
If you have symptoms of emphysema, your doctor will do tests to see how well your lungs work. If you have the condition, you won’t be able to empty your lungs of air as quickly as you should. Doctors call this “airflow limitation.”
Emphysema Types
Emphysema is a type of chronic obstructive pulmonary disease (COPD), and it can be classified into different types, depending on which part of the lungs is affected.
The different types are:
- paraseptal
- centrilobular, affecting mainly the upper lobes; this is most common in smokers
- panlobular, affecting both paraseptal and centrilobular areas
Emphysema Symptoms
You can have emphysema for many years without noticing any signs or symptoms. The main symptom of emphysema is shortness of breath, which usually begins gradually.
You may start avoiding activities that cause you to be short of breath, so the symptom doesn’t become a problem until it starts interfering with daily tasks. Emphysema eventually causes shortness of breath even while you’re at rest.
Symptoms of emphysema may include coughing, wheezing, shortness of breath, chest tightness, and increased production of mucus. Often, symptoms may not be noticed until 50 percent or more of the lung tissue has been destroyed.
Until then, the only symptoms may be a gradual development of shortness of breath and tiredness (fatigue), which can be mistaken for other illnesses. People who develop emphysema have an increased risk of pneumonia, bronchitis, and other lung infections. See your doctor if any of these symptoms arise:
- Shortness of breath, especially during light exercise or climbing steps
- The ongoing feeling of not being able to get enough air
- Long-term cough or “smoker’s cough”
- Wheezing
- Long-term mucus production
- Ongoing fatigue
When to see a doctor
See your doctor if you’ve had unexplained shortness of breath for several months, especially if it’s getting worse or it’s interfering with your daily activities. Don’t ignore it by telling yourself it’s because you’re aging or out of shape. Seek immediate medical attention if:
- You’re so short of breath, you can’t climb stairs
- Your lips or fingernails turn blue or gray with exertion
- You’re not mentally alert
Emphysema Causes
Smoking is the number one factor. Because of this, emphysema is one of the most preventable types of respiratory diseases. Air pollutants in the home and workplace, genetic (inherited) factors (alpha-1 antitrypsin deficiency), and respiratory infections can also play a role in causing emphysema.
Cigarette smoking not only destroys lung tissue, but it also irritates the airways. This causes inflammation and damage to cilia that line the bronchial tubes. This results in swollen airways, mucus production, and difficulty clearing the airways. All of these changes can lead to shortness of breath.
The main cause of emphysema is long-term exposure to airborne irritants, including:
- Tobacco smoke
- Marijuana smoke
- Air pollution
- Chemical fumes and dust
Rarely, emphysema is caused by an inherited deficiency of a protein that protects the elastic structures in the lungs. It’s called alpha-1-antitrypsin deficiency emphysema.
Emphysema Diagnosis
A doctor will carry out a physical examination and ask the patient about their symptoms and medical history.
Some diagnostic tests may also be used, to confirm that the patient has emphysema rather than asthma and heart failure.
If the patient has never smoked, a test may be carried out to see if the person has an α1-antitrypsin deficiency.
The diagnosis of emphysema cannot be made solely on symptoms. Several tests are used to make the diagnosis. One simple test is to tap on your chest and listen with a stethoscope for a hollow sound. This means that air is being trapped in your lungs. Other tests include:
- X-rays: X-rays are generally not useful for detecting the early stages of emphysema. However,
- X-rays can help diagnose moderate or severe cases. Either a plain chest X-ray or a CAT (computer-aided tomography) scan can be used. Once the test is completed, the readings are compared to X-rays of healthy or normal lungs.
- Pulse oximetry: This test is also known as an oxygen saturation test. Pulse oximetry is used to measure the oxygen content of the blood. This is done by attaching the monitor to a person’s finger, forehead, or earlobe.
- Spirometry and pulmonary function tests (PFT): This is one of the most useful tests to determine airway blockage. Spirometry or PFT tests the lungs’ volume by measuring airflow while a patient inhales and exhales. This test is done by taking a deep breath and then blowing into a tube that is hooked up to a specialized machine. These tests are compared to normal results from people of similar gender, age, height, weight, and ethnic background.
- Arterial blood gas: This test measures the amount of oxygen and carbon dioxide in the blood from an artery. It is a test often used as emphysema worsens. It is especially helpful in determining if a patient needs extra oxygen.
- Electrocardiogram (ECG): ECGs check heart function and are used to rule out heart disease as a cause of shortness of breath.
You might also talk to your doctor about whether testing for alpha-1 antitrypsin deficiency is appropriate for you.
Emphysema Stages of Death
The stages of emphysema have been described by the Global Initiative for Chronic Obstructive Lung Disease (GOLD).
The stages are based on forced expiratory volume in 1 second (FEV1).
- Very mild or Stage 1: FEV1 is about 80 percent of normal
- Moderate or Stage 2: FEV1 is between 50 and 80 percent of normal
- Severe or Stage 3: FEV1 is between 30 and 50 percent of normal
- End-stage or stage 4: FEV1 falls below 30%. This is the final stage of COPD, and it will severely affect a person’s daily life.
-
There are two ways to measure end-stage COPD. Clinical symptoms are those that testing at a doctor’s office can reveal.
These symptoms can include:
- low blood oxygen, or hypoxemia
- hypoxia, which is low oxygen in the body’s tissues
- cyanosis, a bluish hue to the skin due to oxygen deprivation
- chronic respiratory failure, which occurs when the respiratory system cannot take in enough oxygen or release enough carbon dioxide
The stages help describe the condition, but they cannot predict how long a person is likely to survive. Doctors can carry out tests to know more about how serious a person’s condition is.
Lung function tests
Lung function tests are used to confirm a diagnosis of emphysema, to monitor disease progression, and to assess response to treatment.
They measure the capacity of the lungs to exchange respiratory gases and include spirometry.
Spirometry assesses airflow obstruction. It takes measurements according to the reduction in forced expiratory volume after bronchodilator treatment.
In this test, patients blow as fast and hard as possible into a tube. The tube is attached to a machine that measures the volume and speed of air blown out.
Forced expiratory volume in one second is abbreviated to FEV.
The four stages of COPD from mild to severe are determined by FEV.
Other tests
Other tests used by doctors in the process of diagnosing COPD and emphysema include:
- imaging, such as a chest X-ray or CT scan of the lungs
- arterial blood gas analysis to assess oxygen exchange
Emphysema Facts & Risk factors
Factors that increase your risk of developing emphysema include:
Smoking. Smoking is one of the major risk factors for developing emphysema; the risk increases as the number of years the person has been smoking increases and is related to the amount of tobacco smoked (for example, three cigarettes a day versus a pack and a half per day); smoking is a major risk factor also for developing lung cancer.
Emphysema is most likely to develop in cigarette smokers, but cigar and pipe smokers also are susceptible. The risk for all types of smokers increases with the number of years and the amount of tobacco smoked.
Age. Although the lung damage that occurs in emphysema develops gradually, most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60.
Exposure to secondhand smoke. Secondhand smoke, also known as passive or environmental tobacco smoke, is smoke that you inadvertently inhale from someone else’s cigarette, pipe, or cigar. Being around secondhand smoke increases your risk of emphysema.
Occupational exposure to fumes or dust. If you breathe fumes from certain chemicals or dust from grain, cotton, wood, or mining products, you’re more likely to develop emphysema. This risk is even greater if you smoke.
Exposure to indoor and outdoor pollution. Breathing indoor pollutants, such as fumes from heating fuel, as well as outdoor pollutants car exhaust, for instance, increases your risk of emphysema.
In the underdeveloped parts of the world, indoor air pollution primarily from open wood flames used for cooking is the primary mechanism for acquiring emphysema.
Complications
People who have emphysema are also more likely to develop:
Collapsed lung (pneumothorax). A collapsed lung can be life-threatening in people who have severe emphysema because the function of their lungs is already so compromised. This is uncommon but serious when it occurs.
Heart problems. Emphysema can increase the pressure in the arteries that connect the heart and lungs. This can cause a condition called cor pulmonale, in which a section of the heart expands and weakens.
Large holes in the lungs (bullae). Some people with emphysema develop empty spaces in the lungs called bullae. They can be as large as half the lung. In addition to reducing the amount of space available for the lung to expand, giant bullae can increase your risk of pneumothorax.
Emphysema Treatment
Treatment of COPD and emphysema aims to stabilize the condition and prevent complications through the use of medication and supportive therapy.
Emphysema can worsen over time and there is no known cure, treatment is focused on slowing the speed of decline. The type of treatment will depend on the severity of the disease.
Quitting smoking: If you smoke, quit. This is the most important step you can take to protect your lungs. It is never too late to quit. Your doctor can help you find the best smoking quitting method for you.
Bronchodilator medications: These medicines relax the muscles around the airways. They are often used to treat asthma. Bronchodilators, given through hand-held inhalants, produce more immediate results and have fewer side effects than oral medications.
Anti-inflammatory medication: These medications reduce inflammation in the airways. However, the long-term side effects of these drugs include osteoporosis, hypertension, high blood sugar, and fat redistribution.
Oxygen therapy: Oxygen therapy is prescribed for patients whose lungs are not getting enough oxygen to the blood (hypoxemia). These patients can’t absorb enough oxygen from the outside air and need to get more oxygen through a machine (a nasal catheter or a facemask).
Lung volume reduction surgery: Lung volume reduction surgery involves removing a portion of diseased lung tissue, then joining together the remaining tissue. Doing this may relieve pressure on the breathing muscles and help improve lung elasticity (or stretch). The results of the surgery have been very promising. Not all patients with emphysema are candidates for this surgery.
Supportive therapy includes oxygen therapy and helps with smoking cessation.
Drug therapies
The main type of medication used for COPD and emphysema are inhaled bronchodilators to relieve symptoms.
These help by relaxing and opening the air passages in the lungs.
Bronchodilators that are supplied through the inhalers include:
- Beta-agonists, which relax bronchial smooth muscle and increase mucociliary clearance
- Anticholinergics, or antimuscarinics, which relax bronchial smooth muscle.
These drugs are equally effective when regularly used to improve lung function and increase exercise capacity.
- There are short-acting and long-acting drugs, and these can be combined.
- The choice depends on individual factors, preferences, and symptoms.
- Examples include albuterol, formoterol, indacaterol, and salmeterol.
Corticosteroid drugs, such as fluticasone, may also help. The steroids are inhaled as an aerosol spray. They can help relieve symptoms of emphysema associated with asthma and bronchitis.
Corticosteroids may help people with poorly controlled symptoms who regularly experience exacerbations despite using a bronchodilator.
In patients who continue to smoke, corticosteroids do not alter the course of the disease, but they can relieve symptoms and improve short-term lung function in some patients.
Used alongside bronchodilators, they can reduce the frequency of attacks.
However, there is a long-term risk of side-effects that include osteoporosis and cataract formation.
Oxygen therapy
As emphysema progresses and respiratory function declines, independent breathing becomes more difficult.
Oxygen therapy improves oxygen delivery to the lungs. Oxygen can be supplemented by using a range of devices, some of them for home use.
Options include electrically driven oxygen concentrators, liquid oxygen systems, or cylinders of compressed gas, depending on needs and how much time the person spends outdoors or at home.
- Oxygen therapy can be administered 24 hours a day or 12 hours at night.
- Oxygen therapy can be administered 24 hours a day or 12 hours at night.
- It prolongs life for people with advanced COPD and emphysema.
- Patients will be monitored for oxygen saturation to prevent oxygen toxicity.
- Air travel may create the need for supplemental oxygen due to the lower flight cabin air pressure.
Surgery
People with severe emphysema sometimes undergo surgery to reduce lung volume or carry out lung transplantation.
Lung volume reduction surgery removes small wedges of the damaged, emphysematous, lung tissue.
This is thought to enhance lung recoil and to improve the function of the diaphragm. In severe cases, this can improve lung function, exercise tolerance, and quality of life.
Lung transplantation improves the quality of life, but not life expectancy, for people with severe emphysema.
Lifelong drug therapy is necessary to prevent the immune system from rejecting the new tissue. One or both lungs may be transplanted.
Treatment of exacerbations
Complications can be managed using drug and oxygen therapy. Antibiotics can help in cases of bacterial infection.
Most exacerbations are treated with corticosteroid drugs, such as prednisone, and oxygen therapy.
Opioid drugs may relieve severe coughing and pain may be relieved by opioid drugs.
In 2014, scientists at the University of Texas Medical Branch in Galveston succeeded in growing human lungs using stem cells. In the future, this could offer hope for people with emphysema and other lung conditions.
Pulmonary rehabilitation and lifestyle management
Pulmonary rehabilitation is a program of care for people with emphysema.
It aims to help people improve their lifestyle by quitting smoking, following a healthy diet, and getting some exercise.
Drinking plenty of water can help keep the airways clear by loosening the mucus.
In winter, avoiding cold air can prevent muscular spasms. A scarf around the mouth or a cold-air face mask may help.
These changes may not alter the overall course of the illness, but they can help people live with the condition, and improve exercise capacity and quality of life.
Exercises that can help improve breathing include diaphragmatic breathing, purse-lip breathing, and deep breathing.
Other Treatments
People with emphysema are often underweight. Eating foods rich in vitamins A, C, and E, like fruits and vegetables, is recommended to improve your overall health.
Getting vaccinated against certain infections, such as pneumonia, can help prevent getting an infection that could complicate emphysema.
People with emphysema often experience anxiety and depression because they aren’t as active as they used to be. In some cases, they may be bound to an oxygen tank. Joining a support group can help you connect with others who have the disease and share similar experiences. This can help you realize that you aren’t alone in fighting the disease.
If you have emphysema, it’s important to know when and where to get help for your symptoms. You should get emergency care if you have severe symptoms, such as trouble catching your breath or talking. Call your health care provider if your symptoms are getting worse or if you have signs of an infection, such as a fever.
Prevention
If you smoke, stop. If you don’t smoke, don’t start. By quitting smoking you can either prevent emphysema or slow its progression.
You also should limit your exposure to air pollution. Restrict your outdoor activity when there are reports of high smog levels.
People exposed to harmful chemicals at work should speak to their employers about respirator masks. Or, consult with a specialist in occupational medicine.
If you have emphysema, ask your doctor about vaccinations against influenza (flu) and pneumococcal pneumonia. These vaccinations can help to prevent life-threatening respiratory infections in people with lung disease.
To prevent emphysema, don’t smoke, and avoid breathing secondhand smoke. Wear a mask to protect your lungs if you work with chemical fumes or dust.
Since emphysema is mainly caused by smoking tobacco, the best way to prevent it is to refrain from smoking. Also, stay away from harmful chemicals and fumes, and heavy pollution.
The outlook for people with emphysema varies based on its severity. There is no cure for the disease, and it gets worse with time, but you can slow its progression. As a rule, smoking cigarettes speeds up the disease, so quitting is important.
Early detection of the disease is important because people with emphysema can develop life-threatening conditions when the lungs and heart become damaged over time.
It’s important to stay healthy by eating well and getting exercise. Quitting smoking is also an important step in the treatment process. With the aid of medications and therapies, you can live a long, healthy life with emphysema.
Vaccination
Vaccination can help prevent COPD and emphysema from getting worse.
Annual flu immunization is required, and a 5-yearly one against pneumonia may be recommended.
Nutrition
Reduced lung capacity places higher energy demand on daily activities, so people with emphysema can be at risk of weight loss and nutritional deficiency.
Some people with emphysema are overweight or obese, and they are encouraged to lose weight, as these conditions can lead to further ill health.
A healthy diet with plenty of fresh fruits, vegetables, and whole grains and a low intake of fat and sugar is important.
0 200



No Comments