Fibromyalgia
Overview
Fibromyalgia is a disorder characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory, and mood issues. Researchers believe that fibromyalgia amplifies painful sensations by affecting the way your brain processes pain signals.
Symptoms sometimes begin after a physical trauma, surgery, infection, or significant psychological stress. In other cases, symptoms gradually accumulate over time with no single triggering event.
Women are more likely to develop fibromyalgia than are men. Many people who have fibromyalgia also have tension headaches, temporomandibular joint (TMJ) disorders, irritable bowel syndrome, anxiety, and depression.
While there is no cure for fibromyalgia, a variety of medications can help control symptoms. Exercise, relaxation, and stress-reduction measures also may help.
What is fibromyalgia?
Fibromyalgia is a long-term (chronic) condition.
It causes:
- pain in the muscles and bones (musculoskeletal pain)
- areas of tenderness
- general fatigue
- sleep and cognitive disturbances
This condition can be hard to understand, even for healthcare providers. Its symptoms mimic those of other conditions, and there aren’t any real tests to confirm the diagnosis. As a result, fibromyalgia is often misdiagnosed.
In the past, some healthcare providers even questioned whether fibromyalgia was real. Today, it is much better understood. Some of the stigma that used to surround it has eased.
Fibromyalgia can still be challenging to treat. But medications, therapy, and lifestyle changes can help you to manage your symptoms and to improve your quality of life.
Fibromyalgia symptoms
Fibromyalgia causes what’s now referred to as “regions of pain.” Some of these regions overlap with what was previously referred to as areas of tenderness called “trigger points” or “tender points.” However, some of these previously noted areas of tenderness have been excluded.
The pain in these regions feels like a consistent dull ache. Your healthcare provider will consider a diagnosis of fibromyalgia if you’ve experienced musculoskeletal pain in 4 out of the 5 regions of pain outlined in the 2016 revisions to the fibromyalgia diagnostic criteria.
This diagnostic protocol is referred to as “multisite pain.” It’s in contrast to the 1990 fibromyalgia diagnostic criteria definition for “chronic widespread pain.”
This process of diagnosis focuses on the areas of musculoskeletal pain and severity of pain as opposed to an emphasis on pain duration, which was the previously the focal criteria for a fibromyalgia diagnosis.
- Widespread pain. The pain associated with fibromyalgia often is described as a constant dull ache that has lasted for at least three months. To be considered widespread, the pain must occur on both sides of your body and above and below your waist.
- Fatigue. People with fibromyalgia often awaken tired, even though they report sleeping for long periods of time. Sleep is often disrupted by pain, and many patients with fibromyalgia have other sleep disorders, such as restless legs syndrome and sleep apnea.
- Cognitive difficulties. A symptom commonly referred to as “fibro fog” impairs the ability to focus, pay attention, and concentrate on mental tasks.
Fibromyalgia often co-exists with other painful conditions, such as:
- Irritable bowel syndrome
- Migraine and other types of headaches
- Interstitial cystitis or painful bladder syndrome
- Temporomandibular joint disorders
Other symptoms of fibromyalgia include:
- fatigue
- trouble sleeping
- sleeping for long periods of time without feeling rested (nonrestorative sleep)
- headaches
- depression
- anxiety
- trouble focusing or paying attention
- pain or a dull ache in the lower belly
- dry eyes
- bladder problems, such as interstitial cystitis
In people with fibromyalgia, the brain and nerves may misinterpret or overreact to normal pain signals. This may be due to a chemical imbalance in the brain or abnormality in the dorsal root ganglionTrusted Source affecting central pain (brain) sensitization.
Fibromyalgia can also affect your emotions and energy level.
Learn which of its symptoms could have the biggest impact on your life.
Fibromyalgia fog
Fibromyalgia fog – also known as “fibro fog” or “brain fog” – is a term some people use to describe the fuzzy feeling they get. Signs of fibro fog include:
- memory lapses
- difficulty concentrating
- trouble staying alert
According to a 2015 study trusted Source published in Rheumatology International, some people find mental fogginess from fibromyalgia more upsetting than pain.
Fibromyalgia Symptoms in females
Fibromyalgia symptoms have generally been more severe in women than in men. Women have more widespread pain, IBS symptoms, and morning fatigue than men. Painful periods are also common.
However, when the 2016 revisions to the diagnostic criteria are applied, more men are being diagnosed with fibromyalgia, which may reduce the degree of distinction between the pain levels men and women experience. More research needs to be done to further evaluate that distinction.
The transition to menopause could make fibromyalgia worse.
Complicating things is the fact that some symptoms of menopause and fibromyalgia look almost identical.
Fibromyalgia in men
Men also get fibromyalgia. Yet, they may remain undiagnosed because this is seen as a woman’s disease. However, current statistics show that as the 2016 diagnostic protocol is more readily applied, more men are being diagnosed.
Men also have severe pain and emotional symptoms from fibromyalgia. The condition affects their quality of life, career, and relationships, according to a 2018 survey published in the American Journal of Public Health.
Part of the stigma and difficulty in getting diagnosed stems from society’s expectation that men who are in pain should “suck it up.”
Men who do venture in to see a doctor can face embarrassment, and the chance that their complaints won’t be taken seriously.
Fibromyalgia trigger points
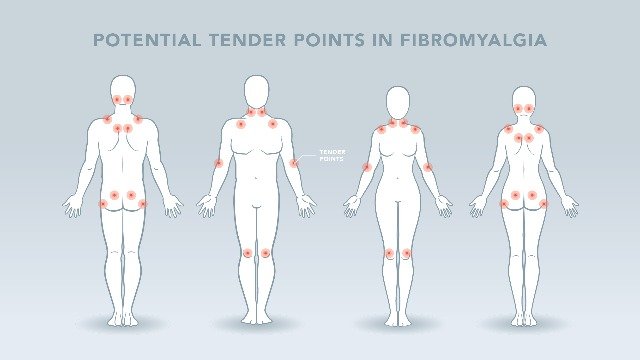
In the past, people were diagnosed with fibromyalgia if they had widespread pain and tenderness in at least 11 out of 18 specific trigger points around their bodies. Healthcare providers would check to see how many of these points were painful by pressing firmly on them.
Common trigger points included the:
- back of the head
- tops of the shoulders
- upper chest
- hips
- knees
- outer elbows
For the most part, trigger points are no longer a part of the diagnostic process.
Instead, healthcare providers may diagnose fibromyalgia if you’ve had pain in 4 out of the 5 areas of pain as defined by the 2016 revised diagnostic criteria, and you have no other diagnosable medical condition that could explain the pain.
Fibromyalgia pain
Pain is the hallmark fibromyalgia symptom. You’ll feel it in various muscles and other soft tissues around your body.
The pain can range from a mild achiness to an intense and almost unbearable discomfort. Its severity could dictate how well you cope from day to day.
Fibromyalgia appears to stem from an abnormal nervous system response. Your body overreacts to things that shouldn’t normally be painful. And you may feel the pain in more than one area of your body.
However, available research still doesn’t pinpoint an exact cause for fibromyalgia. Research continues to evolve in a better understanding of this condition and its origin.
Chest pain
When fibromyalgia pain is in your chest, it can feel frighteningly similar to the pain of a heart attack.
Chest pain in fibromyalgia is actually centered in the cartilage that connects your ribs to your breastbone. The pain may radiate to your shoulders and arms.
Fibromyalgia chest pain may feel:
- sharp
- stabbing
- like a burning sensation
And similar to a heart attack, it can make you struggle to catch your breath.
Back pain
Your back is one of the most common places to feel pain. About 80 percent of Americans have low back pain at some point in their lives. If your back hurts, it may not be clear whether fibromyalgia is to blame, or another condition like arthritis or a pulled muscle.
Other symptoms like brain fog and fatigue can help pinpoint fibromyalgia as the cause. It’s also possible to have a combination of fibromyalgia and arthritis.
The same medications you take to relieve your other fibromyalgia symptoms can also help with back pain. Stretching and strengthening exercises can help provide support to the muscles and other soft tissues of your back.
Leg pain
You can also feel fibromyalgia pain in the muscles and soft tissues of your legs. Leg pain can feel similar to the soreness of a pulled muscle or the stiffness of arthritis. It can be:
- deep
- burning
- throbbing
Sometimes fibromyalgia in the legs feels like numbness or tingling. You may have a creepy crawling sensation. An uncontrollable urge to move your legs is a sign of restless legs syndrome (RLS), which can overlap with fibromyalgia.
Fatigue sometimes manifests in the legs. Your limbs can feel heavy as if they’re held down by weights.
Fibromyalgia causes
Doctors don’t know what causes fibromyalgia, but it most likely involves a variety of factors working together. These may include:
Genetics. Because fibromyalgia tends to run in families, there may be certain genetic mutations that may make you more susceptible to developing the disorder.
Infections. Some illnesses appear to trigger or aggravate fibromyalgia.
Physical or emotional trauma. Fibromyalgia can sometimes be triggered by physical trauma, such as a car accident. Psychological stress may also trigger the condition.
Healthcare providers and researchers don’t know what causes fibromyalgia.
According to the latest research, the cause appears to be a multiple-hit theory that involves genetic disposition (hereditary characteristics) complemented by a trigger, or a set of triggers, such as infection, trauma, and stress.
Let’s take a closer look at these potential factors and several more that may influence why people develop fibromyalgia.
Doctors aren’t sure why some people get fibromyalgia. Many things could cause the body’s pain signals to go awry. Plus, different people report different things that seemed to trigger their condition.
You can even have more than one cause. They can include:
- Genes. Fibromyalgia seems to run in families. Your parents may pass on genes that make you more sensitive to pain. Other genes can also make you more likely to feel anxious or depressed, which makes the pain worse.
- Other diseases. A painful disease like arthritis or an infection raises your chances of getting fibromyalgia.
- Emotional or physical abuse. Children who are abused are more likely to have the condition when they grow up. This may happen because abuse changes the way the brain handles pain and stress.
- Posttraumatic stress disorder (PTSD). Some people have this mental health problem after a terrible event, like war, a car crash, or rape. These events are also linked to fibromyalgia in some people.
- Gender. The condition is much more common in women than in men. Doctors think this could be related to differences in the way men and women feel and react to pain, as well as how society expects them to respond to pain.
- Anxiety and depression. These and other mood disorders seem linked to fibromyalgia, though there’s no proof that they actually cause the condition.
- Not moving enough. The condition is much more common in people who aren’t physically active. Exercise is one of the best treatments for fibromyalgia you already have. It can help turn the pain volume down.
Although Fibromyalgia can affect the quality of life, it is still considered medically benign. It does not cause any heart attacks, stroke, cancer, physical deformities, or loss of life.
Why does it hurt?
Researchers believe repeated nerve stimulation causes the brains of people with fibromyalgia to change. This change involves an abnormal increase in levels of certain chemicals in the brain that signal pain (neurotransmitters). In addition, the brain’s pain receptors seem to develop a sort of memory of the pain and become more sensitive, meaning they can overreact to pain signals.
Infections
A past illness could trigger fibromyalgia or make its symptoms worse. The flu, pneumonia, GI infections, such as those caused by Salmonella and Shigella bacteria, and the Epstein-Barr virus all have possible links to fibromyalgia.
Genes
Fibromyalgia often runs in families. If you have a family member with this condition, you’re at higher risk for developing it.
Researchers think certain gene mutations may play a role. They’ve identified a few possible genes that affect the transmission of chemical pain signals between nerve cells.
Trauma
People who go through severe physical or emotional trauma may develop fibromyalgia. The condition has been linked trusted Source to post-traumatic stress disorder (PTSD).
Stress
Like trauma, stress can leave long-lasting effects on your body. Stress has been linked to hormonal changes that could contribute to fibromyalgia.
Healthcare providers don’t fully understand what causes the chronic widespread nature of fibromyalgia pain. One theory is that the brain lowers the pain threshold. Sensations that weren’t painful before become very painful over time.
Another theory is that the nerves overreact to pain signals.
They become more sensitive, to the point where they cause unnecessary or exaggerated pain.
Fibromyalgia and autoimmunity
In autoimmune diseases like rheumatoid arthritis (RA) or multiple sclerosis (MS), the body mistakenly targets its own tissues with proteins called autoantibodies. Just like it would normally attack viruses or bacteria, the immune system instead attacks the joints or other healthy tissues.
Fibromyalgia symptoms look very similar to those of autoimmune disorders. These symptom overlaps have led to the theory that fibromyalgia could be an autoimmune condition.
This claim has been hard to prove, in part because fibromyalgia doesn’t cause inflammation, and to-date reproducing autoantibodies haven’t been found.
Yet, it’s possible to have an autoimmune disease and fibromyalgia simultaneously.
Fibromyalgia risk factors
Your s**x. Fibromyalgia is diagnosed more often in women than in men.
Family history. You may be more likely to develop fibromyalgia if a relative also has the condition.
Other disorders. If you have osteoarthritis, rheumatoid arthritis, or lupus, you may be more likely to develop fibromyalgia.
Fibromyalgia flare-ups can be the result of:
- stress
- injury
- an illness, such as the flu
An imbalance in brain chemicals may cause the brain and nervous system to misinterpret or overreact to normal pain signals.
Other factors that increase your risk of developing fibromyalgia include:
- Gender. Most fibromyalgia cases are currently diagnosed in women, although the reason for this gender disparity isn’t clear.
- Age. You’re most likely to be diagnosed in middle age, and your risk increases as you get older. However, children can develop fibromyalgia also.
- Family history. If you have close family members with fibromyalgia, you may be at greater risk of developing it.
- Disease. Although fibromyalgia isn’t a form of arthritis, having lupus or RA may increase your risk of also having fibromyalgia.
Complications of fibromyalgia
The pain and lack of sleep associated with fibromyalgia can interfere with your ability to function at home or on the job. The frustration of dealing with an often-misunderstood condition also can result in depression and health-related anxiety.
Fibromyalgia can cause pain, disability, and a lower quality of life. US adults with fibromyalgia may have complications such as:
- More hospitalizations. If you have fibromyalgia you are twice as likely to be hospitalized as someone without fibromyalgia.
- Lower quality of life. Women with fibromyalgia may experience a lower quality of life.
- Higher rates of major depression. Adults with fibromyalgia are more than 3 times more likely to have major depression than adults without fibromyalgia. Screening and treatment for depression are extremely important.
- Higher death rates from suicide and injuries. Death rates from suicide and injuries are higher among fibromyalgia patients, but overall mortality among adults with fibromyalgia is similar to the general population.
- Higher rates of other rheumatic conditions. Fibromyalgia often co-occurs with other types of arthritis such as osteoarthritis, rheumatoid arthritis, systemic lupus erythematosus, and ankylosing spondylitis.
How to diagnose fibromyalgia
Doctors usually diagnose fibromyalgia using the patient’s history, physical examination, X-rays, and blood work.
Your healthcare provider may diagnose you with fibromyalgia if you’ve had widespread pain for 3 months or longer. “Widespread” means the pain is on both sides of your body, and you feel it above and below your waist.
After a thorough examination, your healthcare provider must conclude that no other condition is causing your pain.
No lab test or imaging scan can detect fibromyalgia. Your healthcare provider may use these tests to help rule out other possible causes of your chronic pain.
Fibromyalgia can be hard for healthcare providers to distinguish from autoimmune diseases because the symptoms often overlap.
Some research has pointed to a link between fibromyalgia and autoimmune diseases like Sjogren’s syndrome.
Treatment for Fibromyalgia
Fibromyalgia can be effectively treated and managed with medication and self-management strategies. You can learn about self-management strategies in the section below titled How can I improve my quality of life?
Fibromyalgia should be treated by a doctor or team of healthcare professionals who specialize in the treatment of fibromyalgia and other types of arthritis, called rheumatologists.
Currently, there isn’t a cure for fibromyalgia. Instead, treatment focuses on reducing symptoms and improving quality of life with:
- medications
- self-care strategies
- lifestyle changes
Medications can relieve pain and help you sleep better. Physical and occupational therapy improve your strength and reduce stress on your body. Exercise and stress-reduction techniques can help you feel better, both mentally and physically.
Doctors usually treat fibromyalgia with a combination of treatments, which may include:
- Medications, including prescription drugs and over-the-counter pain relievers.
- Aerobic exercise and muscle-strengthening exercise.
- Patient education classes, usually in primary care or community settings.
- Stress management techniques such as meditation, yoga, and massage.
- Good sleep habits to improve the quality of sleep.
- Cognitive-behavioral therapy (CBT) to treat the underlying depression. CBT is a type of talk therapy meant to change the way people act or think.
In addition to medical treatment, people can manage their fibromyalgia with the self-management strategies described below, which are proven to reduce pain and disability, so they can pursue the activities important to them.
In addition, you may wish to seek out support and guidance. This may involve seeing a therapist or joining a support group.
In a support group, you can get advice from other people who have fibromyalgia to help you through your own journey.
Physical therapies
Depending on how your fibromyalgia is affecting you, your doctor may refer you to a physiotherapist or occupational therapist.
Physiotherapy
Physiotherapy can help relieve the pain of fibromyalgia.
Physiotherapists are trained specialists who can help you stay active and independent. They will show you the best exercises to strengthen your muscles, without hurting yourself or putting your body under too much strain.
They can show you how something as simple as improving your posture can help your pain. They may also advise you on relaxation techniques which can be just as important as exercise when you’re dealing with fibromyalgia.
Your doctor can refer you to an NHS physiotherapist. In some areas, you can refer yourself, but this may take a while.
It can be quicker to see a physiotherapist privately, but you would pay for the appointment. To find a private physiotherapist, visit the Chartered Society of Physiotherapy website.
Occupational therapy
Occupational therapy can help you manage your everyday activities around your fibromyalgia, without increasing your pain or overwhelming yourself.
Your occupational therapist may suggest new ways you can get things done. They may also teach you some relaxation techniques.
If you still find some activities difficult after you’ve made these changes, they may suggest equipment, known as aids and adaptations, to help you.
Your doctor can refer you to an occupational therapist or you can see one privately, for a fee.
If you’re having problems at work, your employer may have an occupational health team that could help you. Otherwise, you can contact a Jobcentre Plus office to ask for advice.
Pain clinics and pain management programs
Pain clinics bring together the skills of a wide range of professionals, such as:
- specialist pain consultants
- physiotherapists
- occupational therapists
- psychologists
- social workers
- employment advisors.
They can provide specific treatments or rehabilitation therapies that could reduce the effects of fibromyalgia.
A pain specialist may suggest you join a pain management program, which brings together people with different long-term pain conditions. Pain management won’t take away your pain, but it can help you manage it better and reduce its impact on your life.
These sessions are often led by psychologists who specialize in helping people find ways to live with their pain. They are usually held in an outpatient clinic and run over several days or weeks.
Psychological therapies
Pain is never just a physical experience, especially if it lasts a long time. Pain can affect your mood and behavior.
Psychological approaches to pain management try to address the emotional effects of your pain and the things that can make your pain worse.
They help you look at how your pain affects your thoughts and habits, and how your emotions can affect your pain.
Therapies such as cognitive-behavioral therapy (CBT), which is a talking therapy, try to reduce the overwhelming effect of problems such as stress, unhappiness, and pain.
They aim to help you understand how you react to different problems by breaking them down into smaller, more manageable, chunks. This should help you change the way you react to them and the effect they have on you.
Making small changes to the way you react to a situation or problem can often improve both your emotional and physical health.
Psychological therapies can also include relaxation techniques and other ways to reduce your stress.
They encourage you not to be too hard on yourself, even when you feel frustrated, and to accept that sometimes there are limits to what you can do.
A number of healthcare professionals often have training in CBT, so you may not have to see a psychologist.
For more information about psychological therapies and CBT, the British Association for Behavioural & Cognitive Psychotherapies (BABCP) keeps a register of all accredited therapists in the UK.
Drug treatments
Your doctor can prescribe medications to help with the pain, sleep problems, or depression you may be experiencing because of your fibromyalgia.
Drugs can’t treat fibromyalgia alone, but they can help reduce your symptoms to a level that will allow you to start some gentle physical activity and rehabilitation therapies.
All drugs have potential side effects. It’s important to talk to your doctor about how to get the best balance between pain relief and any unpleasant effects.
If you feel like treatment isn’t helping you, talk to your doctor.
Neuromodulatory drugs
These are prescribed treatments, such as antidepressants, or drugs targeting nerve pain, including pregabalin and gabapentin. They were originally used to treat conditions such as depression and epilepsy but have since proved effective for treating fibromyalgia.
They work by changing how the brain and central nervous system process pain.
Antidepressant drugs
Antidepressants, such as amitriptyline or nortriptyline, can reduce pain and help you sleep. When used to treat pain they are prescribed at a lower dose compared to when they are used to treat depression. They can, however, still help with the low mood at this lower dose.
Some people say certain types, such as duloxetine, help relieve pain and other symptoms.
Some antidepressants can make you feel sleepy, so avoid taking them before you drive, cycle, or use heavy machinery. You usually need to take them about two hours before bedtime.
You might need to take them for a few months before you feel their full benefits. Your doctor will gradually increase the dose to a level that works for you.
Pregabalin and gabapentin
Pregabalin and gabapentin are used to treat nerve pain and have been shown to help some people with fibromyalgia.
You are likely to be started on a low dose and, depending on how you respond to them, it will be increased gradually to a level that works for you.
They can cause side effects such as drowsiness, dizziness, and weight gain, and it may take six weeks before you see any real differences in your pain.
Pregabalin and gabapentin are classed as controlled substances and will only be prescribed one month at a time.
- Painkillers
- Paracetamol
- Paracetamol can ease the pain for some people with fibromyalgia but doesn’t work for everybody.
Some people find drugs like co-codamol or co-dydramol help. These contain paracetamol and a low dose of a stronger opioid painkiller.
Co-codamol contains the opioid codeine and co-dydramol is made from an opioid called dihydrocodeine.
Opioid-based painkillers can cause a number of side effects. They are only recommended for short-term use – usually no more than three days. This is because there is a risk people could become addicted to them.
Opioids tend to mask pain and not resolve the problem causing it. There is evidence that long-term use of opioids may actually increase your pain because your body can build up a tolerance to them.
Tramadol
There have been a few small studies that show a drug called tramadol helps. Tramadol works partly as an opioid and partly as an antidepressant. However, your doctor may feel other drug treatments are safer and would help your condition more.
Tramadol is a controlled drug only available on prescription for short-term flare-ups. It can be addictive and people who take it are carefully monitored.
How can I help myself?
Exercise
If you’re in pain, your instinct may be to avoid exercise or moving around too much. But keeping active is a really important part of the treatment for fibromyalgia and can prevent other health problems.
Your symptoms and general health can be improved by a combination of aerobic exercise and movements that improve your flexibility and strength.
Exercise has been proven to improve fatigue and our ability to control pain.
At first, you may find that your pain and tiredness become worse, particularly if you’re starting to exercise muscles that haven’t been used for a while. Try to do the same amount of exercise each day, so you build up your muscle strength and your stamina.
Then, after doing your routine of exercises for a couple of weeks, slowly increase the amount you do, and this will improve your fitness, stamina, and flexibility.
Aerobic exercises
Aerobic exercise is anything that makes you a little out of breath and your heart beat faster.
Swimming is recommended for people with fibromyalgia. Taking a brisk walk and cycling can also help.
At home, you could step up and down your bottom step several times, or march on the spot to get your heart beating faster.
Strengthening exercises
Strengthening exercises help develop and build the muscles that move and protect your joints. They may be difficult at first but should become easier with practice.
Aim to do at least one session a day, either at home or in a gym. Ask a GP or physiotherapist for examples of strengthening exercises you could do at home.
You can also buy specially designed equipment, such as ankle weights. Begin with lighter weights, then move on to heavier ones, if you feel able to.
Strengthening equipment in a gym allows you to work your muscles by pushing or pulling against a resistance, such as weights or elastic ropes. You can ask an instructor for advice about using the equipment if you’re not sure.
Stretching exercises
Stretching, or range of movement, exercises can increase your flexibility. You can do these anywhere. There are plenty of examples of exercises online, or you could ask a physiotherapist. Some people with fibromyalgia have found Tai chi and yoga help.
Diet and nutrition
There’s no particular diet that’s been proven to help fibromyalgia. However, it’s recommended that you keep to a healthy weight by eating a balanced diet that is low in saturated fats, sugar, and salt, and has plenty of fruit and vegetables. It’s also good to drink six to eight glasses of water every day.
Complementary treatments
Some people with fibromyalgia find that complementary treatments help their symptoms.
Acupuncture, where special needles are inserted into the skin above pressure points, may help your pain for a short time. Massage can also be helpful for some people with fibromyalgia. However, the effects don’t often last that long.
If you want to try a complementary treatment, speak to your doctor first, in case it affects any other treatment you’re on.
It’s important to go to a legally registered therapist or one who has a set ethical code and is fully insured.
If you decide to try therapies or supplements, you should be critical of what they’re doing for you and only continue if they’re helping.
Sleep
Poor sleep appears to be a significant cause of fibromyalgia, so getting enough good-quality sleep is an important part of your treatment. Not only will it help with tiredness and fatigue, but it may also improve your pain.
Sleeping tablets are not normally recommended, as the body can become tolerant to them, which can lead to the effects of wearing off and even addiction. But regular activity, particularly aerobic exercise, and cognitive-behavioral therapy (CBT) have proven effective for people with disrupted sleep patterns.
It can also help to change your habits around bedtime. To help you get a better night’s sleep:
- Make sure your bedroom is dark, quiet, and comfortable temperature.
- Try a warm bath before bedtime to help ease pain and stiffness.
- Develop a regular routine, where you go to bed and get up at a similar time each day.
- You may like to try listening to some soothing music before going to bed.
- Some gentle exercises may help reduce muscle tension, but it’s probably best to avoid energetic exercise too close to bedtime.
- Keep a notepad by your bed – if you think of something you need to do the next day, write it down and then put it out of your mind.
- Avoid caffeine in the eight hours before you go to bed.
- Don’t drink alcohol close to bedtime.
- Avoid eating main meals close to bedtime.
- If you smoke, try to stop smoking, or at least don’t smoke close to bedtime.
- Try not to sleep during the day.
- Avoid watching TV and using computers, tablets or smartphones in your bedroom.
- Don’t keep checking the time during the night.
Fibromyalgia medication
The goal of fibromyalgia treatment is to manage pain and improve quality of life. This is often accomplished through a two-pronged approach of self-care and medication.
Common medications for fibromyalgia include:
Pain relievers
Over-the-counter pain relievers such as ibuprofen (Advil) or acetaminophen (Tylenol) can help with mild pain.
Narcotics, such as tramadol (Ultram), which is an opioid, were previously prescribed for pain relief. However, research has shown they’re not effective. Also, the dosage for narcotics is typically increased rapidly, which can pose a health risk for those prescribed these drugs.
Most healthcare providers recommend avoiding narcotics to treat fibromyalgia.
Antidepressants
Antidepressants such as duloxetine (Cymbalta) and milnacipran HCL (Savella) are sometimes used to treat pain and fatigue from fibromyalgia. These medications may also help improve sleep quality and work on rebalancing neurotransmitters.
Antiseizure drugs
Gabapentin (Neurontin) was designed to treat epilepsy, but it may also help reduce symptoms in people with fibromyalgia. Pregabalin (Lyrica), another anti-seizure drug, was the first drug FDA-approved for fibromyalgia. It blocks nerve cells from sending out pain signals.
A few drugs that aren’t FDA-approved to treat fibromyalgia, including antidepressants and sleep aids, can help with symptoms. Muscle relaxants, which were once used, are no longer recommended.
Researchers are also investigating a few experimental treatments that may help people with fibromyalgia in the future.
Fibromyalgia natural remedies
If the medications your healthcare provider prescribes don’t entirely relieve your fibromyalgia symptoms, you can look for alternatives. Many natural treatments focus on lowering stress and reducing pain. You can use them alone or together with traditional medical treatments.
Natural remedies for fibromyalgia include:
- physical therapy
- acupuncture
- 5-hydroxytryptophan (5-HTP)
- meditation
- yoga, use with caution if hypermobility is present
- tai chi
- exercise
- massage therapy
- a balanced, healthy diet
Therapy can potentially reduce the stress that triggers fibromyalgia symptoms and depression.
Group therapy may be the most affordable option, and it will give you a chance to meet others who are going through the same issues.
Cognitive-behavioral therapy (CBT) is another option that can help you manage stressful situations. Individual therapy is also available if you prefer one-on-one help.
It’s important to note that most alternative treatments for fibromyalgia haven’t been thoroughly studied or proven effective.
Ask your healthcare provider about the benefits and risks before trying any of these treatments.
Fibromyalgia diet recommendations
Some people report that they feel better when they follow a specific diet plan or avoid certain foods. But research hasn’t proven that anyone diet improves fibromyalgia symptoms.
If you’ve been diagnosed with fibromyalgia, try to eat a balanced diet overall. Nutrition is important in helping you to keep your body healthy, to prevent symptoms from getting worse, and to provide you with a constant energy supply.
Dietary strategies to keep in mind:
- Eat fruits and vegetables, along with whole grains, low-fat dairy, and lean protein.
- Drink plenty of water.
- Eat more plants than meat.
- Reduce the amount of sugar in your diet.
- Exercise as often as you can.
- Work toward achieving and maintaining your healthy weight.
You may find that certain foods make your symptoms worse, such as gluten or MSG. If that’s the case, keep a food diaryTrusted Source where you track what you eat and how you feel after each meal.
Share this diary with your healthcare provider.
They can help you identify any foods that aggravate your symptoms. Avoiding these foods can be beneficial in helping you manage your symptoms.
Fibromyalgia can leave you feeling tired and worn out.
A few foods will give you the energy boost you need to get through your day.
Fibromyalgia pain relief
Fibromyalgia pain can be uncomfortable and consistent enough to interfere with your daily routine. Don’t just settle for pain. Talk to your healthcare provider about ways to manage it.
One option is to take pain relievers such as:
- aspirin
- ibuprofen
- naproxen sodium
- help with discomfort
- lower pain levels
- help you better manage your condition
These medications bring down inflammation. Though inflammation is not a primary part of fibromyalgia, it may be present as an overlap with RA or another condition. Pain relievers may help you sleep better.
Please note that NSAIDs do have side effects. Caution is advised if NSAIDs is used for an extended period of time as is usually the case in managing a chronic pain condition.
Talk with your healthcare provider to create a safe treatment plan that works well in helping you manage your condition.
Antidepressants and anti-seizure drugs are two other medication classes your healthcare provider may prescribe to manage your pain.
The most effective pain reliever does not come in a medication bottle.
Practices like yoga, acupuncture, and physical therapy can:
Fibromyalgia fatigue can be just as challenging to manage as pain.
Learn a few strategies to help you sleep better and feel more alert during the day.
Living with fibromyalgia
Your quality of life can be affected when you live with pain, fatigue, and other symptoms on a daily basis. Complicating things are the misunderstandings many people have about fibromyalgia. Because your symptoms are hard to see, it’s easy for those around you to dismiss your pain as imaginary.
Know that your condition is real. Be persistent in your pursuit of a treatment that works for you. You may need to try more than one therapy or use a few techniques in combination before you start to feel better.
Lean on people who understand what you’re going through, like:
- your healthcare provider
- close friends
- a therapist
Be gentle on yourself. Try not to overdo it. Most importantly, have faith that you can learn to cope with and manage your condition.
Fibromyalgia Facts and statistics
Fibromyalgia is a chronic condition that causes:
- widespread pain
- fatigue
- difficulty sleeping
- depression
Currently, there’s no cure, and researchers don’t fully understand what causes it. Treatment focuses on medications and lifestyle changes to help ease the symptoms.
About 4 million AmericansTrusted Source ages 18 and over, or about 2 percent of the population, have been diagnosed with fibromyalgia. Most fibromyalgia cases are diagnosed in women, but men and children can also be affected.
Most people get diagnosed in middle age.
Fibromyalgia is a chronic (long-term) condition. However, some people may experience remission-type periods in which their pain and fatigue improve.
Are there any home remedies for fibromyalgia?
The non-medication treatments for fibromyalgia are the cornerstone of the treatment of the syndrome. These include lifestyle changes like education, stress reduction, improving sleep, and exercise.
What is the prognosis of fibromyalgia?
The overall mortality is not increased in patients with fibromyalgia, and it is not an organ-threatening disease. However, many patients with fibromyalgia continue to suffer from long-term widespread pain. Once the diagnosis is confirmed, many fibromyalgia patients find their overall sense of well-being and their pain improves to pain levels that are more moderate with the treatments discussed above.
There are some patients who experience a dramatic reduction in pain with changes in their life to reduce stress. However, these patients are always at risk for worsening of their symptoms in the future and should maintain efforts for a healthy lifestyle, including sleep hygiene, ongoing exercise, and stress management.
Fibromyalgia patients have a higher rate of disability than the general population, but seeking permanent disability status is generally discouraged because it frequently leads to worsening of symptoms.
Is it possible to prevent fibromyalgia?
Fibromyalgia is a syndrome with a genetic predisposition. It can be triggered by certain events, but the exact events leading to the onset of fibromyalgia is unknown. Because of this, there is no known way to prevent fibromyalgia. However, leading a healthy lifestyle, including getting enough sleep, eating healthy foods, and exercising, is the best way to stay healthy.
What is the latest research on fibromyalgia?
There is ongoing medical research on fibromyalgia on many fronts. There is active research on the genes responsible for fibromyalgia, new medications, and new non-medication therapies to help the pain. One recent study found that non-restorative sleep — when one wakes up feeling tired after a full night of sleep — is strongly tied to developing widespread pain. Medical researchers have linked anxiety to developing widespread pain.
How can I improve my quality of life?
Get physically active.
Experts recommend that adults be moderately physically active for 150 minutes per week. Walk, swim, or bike 30 minutes a day for five days a week. These 30 minutes can be broken into three separate ten-minute sessions during the day.
Regular physical activity can also reduce the risk of developing other chronic diseases such as heart disease and diabetes. Learn more about physical activity for arthritis. You can exercise on your own or participate in a CDC-recommended physical activity program.
Go to recommended physical activity programs.
Those concerned about how to safely exercise can participate in physical activity programs that are proven effective for reducing pain and disability related to arthritis and improving mood and the ability to move. Classes take place at local Ys, parks, and community centers. These classes can help you feel better. Learn more about CDC-recommended physical activity programs.
Join a self-management education class,
which helps people with arthritis or other conditions—including fibromyalgia be more confident in how to control their symptoms, how to live well, and understand how the condition affects their lives. Learn more about the CDC-recommended self-management education programs.
0 200



No Comments