Gastroenteritis
Overview
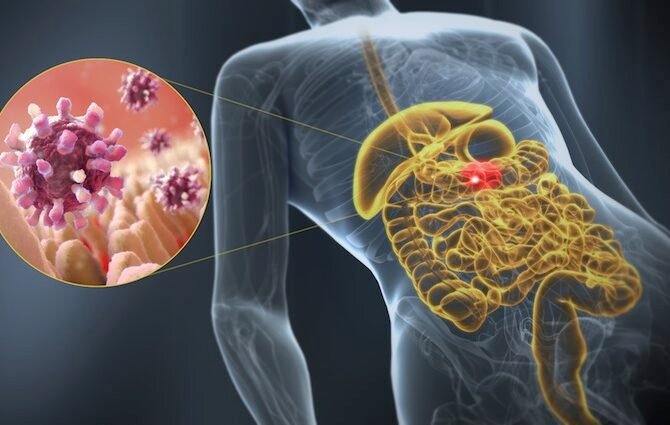
Viral gastroenteritis is an intestinal infection marked by watery diarrhea, abdominal cramps, nausea or vomiting, and sometimes fever.
The most common way to develop viral gastroenteritis often called stomach flu is through contact with an infected person or by ingesting contaminated food or water. If you’re otherwise healthy, you’ll likely recover without complications. But for infants, older adults, and people with compromised immune systems, viral gastroenteritis can be deadly.
There’s no effective treatment for viral gastroenteritis, so prevention is key. In addition to avoiding food and water that may be contaminated, thorough and frequent hand-washings are your best defense.
Gastroenteritis
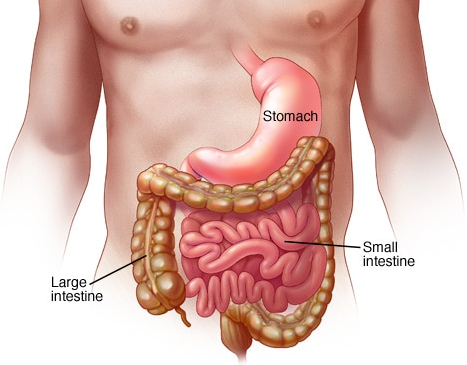
Gastroenteritis, also known as infectious diarrhea and gastro, is inflammation of the gastrointestinal tract the stomach, and the small intestine. Symptoms may include diarrhea, vomiting, and abdominal pain. Fever, lack of energy, and dehydration may also occur. This typically lasts less than two weeks. It is not related to influenza, though it has erroneously been called the “stomach flu”.
Gastroenteritis is usually caused by viruses. However, bacteria, parasites, and fungus can also cause gastroenteritis. In children, rotavirus is the most common cause of severe disease. In adults, nor virus and Campylobacter are common causes. Eating improperly prepared food, drinking contaminated water or close contact with a person who is infected can spread the disease. Treatment is generally the same with or without a definitive diagnosis, so testing to confirm is usually not needed.
Prevention includes handwashing with soap, drinking clean water, breastfeeding babies instead of using the formula, and proper disposal of human waste. The rotavirus vaccine is recommended as a prevention for children. Treatment involves getting enough fluids. For mild or moderate cases, this can typically be achieved by drinking oral rehydration solution (a combination of water, salts, and sugar).
In those who are breastfed, continued breastfeeding is recommended. For more severe cases, intravenous fluids may be needed. Fluids may also be given by a nasogastric tube. Zinc supplementation is recommended in children. Antibiotics are generally not needed. However, antibiotics are recommended for young children with fever and bloody diarrhea.
In 2015, there were two billion cases of gastroenteritis, resulting in 1.3 million deaths globally. Children and those in the developing world are affected the most. In 2011, there were about 1.7 billion cases, resulting in about 700,000 deaths of children under the age of five. In the developing world, children less than two years of age frequently get six or more infections a year. It is less common in adults, partly due to the development of immunity.
It is a common condition, mainly because the microbes that can cause gastroenteritis are easily spread via contaminated food or water and through person-to-person contact. The infection causes the digestive tract to become irritated, which results in diarrhea and other symptoms such as vomiting and abdominal pain and cramping.
Stomach Flu
When you have diarrhea and vomiting, you may say you have the “stomach flu.” These symptoms often are due to a condition called gastroenteritis.
With gastroenteritis, your stomach and intestines are irritated and inflamed. The cause is typically a viral or bacterial infection.
Children can get dehydrated quickly, so if your child has the stomach flu, it’s important that you look for signs that he is very thirsty or has dry skin or a dry mouth. If you have a baby, look for fewer, drier diapers.
Keep children with gastroenteritis out of daycare or school until all symptoms are gone. Check with your doctor before giving your child any medicine. Drugs used to control diarrhea and vomiting aren’t usually given to children younger than 5.
To help prevent rotavirus the most common cause of stomach flu for children — there are two vaccines that can be given to infants. Talk to your doctor about the vaccines.
Gastroenteritis is the irritation of the digestive tract caused by a viral, bacterial, or parasitic infection. Symptoms include diarrhea, vomiting, and abdominal pain. Treatment mainly involves symptom relief and fluid replacement. Gastroenteritis is also known as a tummy bug, stomach flu, intestinal flu, food poisoning, and traveler’s diarrhea.
Signs and symptoms
Gastroenteritis usually involves both diarrhea and vomiting. Sometimes, only one or the other is present. This may be accompanied by abdominal cramps. Signs and symptoms usually begin 12–72 hours after contracting the infectious agent. If due to a virus, the condition usually resolves within one week. Some viral infections also involve fever, fatigue, and headache, and muscle pain. If the stool is bloody, the cause is less likely to be viral and more likely to be bacterial. Some bacterial infections cause severe abdominal pain and may persist for several weeks.
With gastroenteritis, the main symptoms you probably have are watery diarrhea and vomiting. You might also have stomach pain, cramping, fever, nausea, and a headache.
Because of diarrhea and vomiting, you also can become dehydrated. Watch for signs of dehydration, such as dry skin and a dry mouth, feeling lightheaded, and being really thirsty. Call your doctor if you have any of these symptoms.
Children infected with rotavirus usually make a full recovery within three to eight days. However, in poor countries treatment for severe infections is often out of reach and persistent diarrhea is common. Dehydration is a common complication of diarrhea. Severe dehydration in children may be recognized if the skin color and position returns slowly when pressed.
This is called “prolonged capillary refill” and “poor skin turgor”. Abnormal breathing is another sign of severe dehydration. Repeat infections are typically seen in areas with poor sanitation and malnutrition. Stunted growth and long-term cognitive delays can result.
Although it’s commonly called stomach flu, gastroenteritis isn’t the same as influenza. Real flu (influenza) affects only your respiratory system your nose, throat, and lungs. Gastroenteritis, on the other hand, attacks your intestines, causing signs and symptoms, such as:
- Watery, usually nonbloody diarrhea — bloody diarrhea usually means you have a different, more severe infection
- Abdominal cramps and pain
- Nausea, vomiting or both
- Occasional muscle aches or headache
- Low-grade fever
Depending on the cause, viral gastroenteritis symptoms may appear within one to three days after you’re infected and can range from mild to severe. Symptoms usually last just a day or two, but occasionally they may persist as long as 10 days.
Because the symptoms are similar, it’s easy to confuse viral diarrhea with diarrhea caused by bacteria, such as Clostridium difficult, salmonella, and E. coli, or parasites, such as giardia.
The Main Symptom of Gastroenteritis:
Gastroenteritis is diarrhea, which is when your bowel movements (feces or stools) become watery and you need to go to the toilet frequently and urgently. Although diarrhea is the primary symptom of gastroenteritis, there are many other causes of diarrhea. Additional symptoms and signs of gastroenteritis may include:
- Nausea and vomiting
- Abdominal pain and cramping
- Mild fever and chills
- Loss of appetite
- Headache and muscle aches
- Tiredness and general body weakness
- Incontinence (loss of control over bowel motions)
- Poor feeding in infants.
Depending on the cause, symptoms may appear within one to three days after infection and can range from mild to severe. Symptoms usually last one or two days, but occasionally may persist for up to ten days.
You should see your doctor if your symptoms last more than about five days and/or increase in severity, your symptoms go away but come back, your stools become bloody or pussy, you have constant abdominal pain, or if you develop dehydration. Dehydration can arise from the excessive loss of fluid from the body, which can occur quickly with gastroenteritis. The signs and symptoms of dehydration include:
- Extreme thirst
- Not having urinated in the past eight hours or passing only a small volume of urine
- Urine that is dark in color and smelly
- Dry lips and mouth, and a lack of tears
- Cold hands and feet
- Sunken cheeks or eyes
- Dizziness, lethargy, floppiness
- In infants, dry nappies (for longer than 4-6 hours) and/or a sunken fontanelle (the soft spot on the top of a baby’s head)
- Skin that ‘tents up’ when pinched.
Signs of dehydration in anyone, especially infants and children, the elderly, and people with weakened immune systems, are reasons to see a doctor immediately.
How is the stomach flu (gastroenteritis) spread?
Most viral and bacterial causes of the stomach flu can be transferred to other people by direct and indirect contact, usually by the fecal-oral route.
- Direct contact could involve an infant’s hand touching feces-contaminated surfaces and then touching a sibling or relative; indirect contact would be like touching a doorknob or railing on a cruise ship or in a dorm that is contaminated and the person touches the contaminated surface and transfers the agent by touching their mouth.
- Another common way to get stomach flu is drinking or eating contaminated foods and liquids.
Cause
Viruses (particularly rotavirus) and the bacteria Escherichia coli and Campylobacter species are the primary causes of gastroenteritis. There are, however, many other infectious agents that can cause this syndrome including parasites and fungus. Non-infectious causes are seen on occasion, but they are less likely than a viral or bacterial cause. The risk of infection is higher in children due to their lack of immunity. Children are also at higher risk because they are less likely to practice good hygiene habits. Children living in areas without easy access to water and soap are especially vulnerable.
There are many ways gastroenteritis can be spread:
- Contact with someone who has the virus
- Contaminated food or water
- Unwashed hands after going to the bathroom or changing a diaper
The most common cause of gastroenteritis is a virus.
There are main 4 types of viruses.
Rotavirus is the world’s most common cause of diarrhea in infants and young children. Norovirus is the most common cause of serious gastroenteritis and also foodborne disease outbreaks in the U.S.
You’re most likely to contract viral gastroenteritis when you eat or drink contaminated food or water, or if you share utensils, towels, or food with someone who’s infected.
A number of viruses can cause gastroenteritis, including:
Norovirus
Both children and adults are affected by norovirus, the most common cause of foodborne illness worldwide. Norovirus infection can sweep through families and communities. It’s especially likely to spread among people in confined spaces. In most cases, you pick up the virus from contaminated food or water, although person-to-person transmission also is possible.
Norovirus is highly contagious and can affect anyone at any age. It’s spread through contaminated food, water, and surfaces, or by people who have the virus. Norovirus is common in crowded spaces.
Symptoms include:
- nausea
- diarrhea
- fever
- body aches
According to the Centers for Disease Control and Prevention (CDC)Trusted Source, most people with norovirus feel better within one to three days of experiencing symptoms.
Norovirus is the leading cause trusted Source of gastroenteritis in the United States and worldwide. Most outbreaks in the United States occur between November and AprilTrusted Source.
Rotavirus.
Worldwide, this is the most common cause of viral gastroenteritis in children, who are usually infected when they put their fingers or other objects contaminated with the virus into their mouths. The infection is most severe in infants and young children. Adults infected with rotavirus may not have symptoms, but can still spread the illness — of particular concern in institutional settings because infected adults unknowingly can pass the virus to others. A vaccine against viral gastroenteritis is available in some countries, including the United States, and appears to be effective in preventing the infection.
Rotavirus commonly affects infants and young children. They can then spread the infection to other children and adults. It’s usually contracted and transmitted through the mouth.
Symptoms typically appear within two days of infection and include:
- vomiting
- loss of appetite
- watery diarrhea lasting anywhere from three to eight days
According to the CDC, this virus is most common between the months of December and JuneTrusted Source.
A rotavirus vaccine was approved for infants in 2006. Early vaccination is recommended to prevent severe rotavirus illnesses in infants and small children.
Adenovirus
The adenovirus affects people of all ages. It can cause several conditions, including gastroenteritis.
Adenovirus is contracted through the air via sneezing and coughing, by touching contaminated objects, or by touching the hands of someone with the virus.
Symptoms associated with adenovirus include:
- sore throat
- pink eye
- fever
- coughing
- runny nose
Children in daycare, especially those ages 6 months to 2 years, are more likely to get adenovirus.
Most children will feel better within a few days of experiencing adenovirus symptoms. However, symptoms such as pink eye may take longer to go away.
Astrovirus
Astrovirus is another virus that commonly causes gastroenteritis in children. Symptoms associated with astrovirus include:
- diarrhea
- headache
- mild dehydration
- stomach pain
The virus usually affects people in late winter and early spring. It’s passed through contact with a person who has the virus or an infected surface or food.
Although not as common, bacteria such as E. coli and salmonella can also trigger the stomach flu. Salmonella and campylobacter bacteria are the most common bacterial causes of gastroenteritis in the U.S. and are usually spread by undercooked poultry, eggs, or poultry juices. Salmonella can also be spread through pet reptiles or live poultry.
Another bacteria, shigella, is often passed around in daycare centers. It typically is spread from person to person, and common sources of infection are contaminated food and drinking water.
Parasites can also cause gastroenteritis, but it’s not common. You can pick up organisms such as giardia and cryptosporidium in contaminated swimming pools or by drinking contaminated water.
There are also other unusual ways to get gastroenteritis:
- Heavy metals (arsenic, cadmium, lead, or mercury) in drinking water
- Eating a lot of acidic foods, like citrus fruit and tomatoes
- Toxins that might be found in certain seafood
- Medications such as antibiotics, antacids, laxatives, and chemotherapy drugs
Some shellfish, especially raw or undercooked oysters, also can make you sick. Although contaminated drinking water is a cause of viral diarrhea, in many cases the virus is passed through the fecal-oral route that is, someone with a virus handles the food you eat without washing his or her hands after using the toilet.
Viral Gastroenteritis
Rotavirus, norovirus, adenovirus, and astrovirus are known to cause viral gastroenteritis. Rotavirus is the most common cause of gastroenteritis in children and produces similar rates in both the developed and developing world. Viruses cause about 70% of episodes of infectious diarrhea in the pediatric age group. Rotavirus is a less common cause in adults due to acquired immunity. Norovirus is the cause in about 18% of all cases.
Viral gastroenteritis is an inflammation of your stomach and intestines caused by one of any number of viruses. Also known as stomach flu, viral gastroenteritis affects people throughout the world.
Viral gastroenteritis is an inflammation of your stomach and intestines caused by one of any number of viruses. Also known as stomach flu, viral gastroenteritis affects people throughout the world.
This highly contagious illness spreads through close contact with people who are infected or through contaminated food or water.
It can easily spread in close quarters, such as:
- child care facilities
- schools
- nursing homes
- cruise ships
Different viruses can cause the illness, each with their own peak season. The most common viruses include norovirus and rotavirus.
There are steps you can take to lower your chances of contracting the viruses that cause viral gastroenteritis. These include frequent hand-washing and avoiding contaminated water and food products.
Norovirus is the leading cause of gastroenteritis among adults in America, causing greater than 90% of outbreaks. These localized epidemics typically occur when groups of people spend time in close physical proximity to each other, such as on cruise ships, in hospitals, and in restaurants. People may remain infectious even after their diarrhea has ended. Norovirus is the cause of about 10% of cases in children.
Bacterial
in the developed world Campylobacter jejuni is the primary cause of bacterial gastroenteritis, with half of these cases associated with exposure to poultry. In children, bacteria are the cause in about 15% of cases, with the most common types being Escherichia coli, Salmonella, Shigella, and Campylobacter species. If food becomes contaminated with bacteria and remains at room temperature for a period of several hours, the bacteria multiply and increase the risk of infection in those who consume the food.
Some foods commonly associated with the illness include raw or undercooked meat, poultry, seafood, and eggs; raw sprouts; unpasteurized milk and soft cheeses; and fruit and vegetable juices. In the developing world, especially sub-Saharan Africa and Asia, cholera is a common cause of gastroenteritis. This infection is usually transmitted by contaminated water or food.
Toxigenic Clostridium difficult is an important cause of diarrhea that occurs more often in the elderly. Infants can carry these bacteria without developing symptoms. It is a common cause of diarrhea in those who are hospitalized and is frequently associated with antibiotic use. Staphylococcus aureus infectious diarrhea may also occur in those who have used antibiotics.
Acute “traveler’s diarrhea” is usually a type of bacterial gastroenteritis, while the persistent form is usually parasitic. Acid-suppressing medication appears to increase the risk of significant infection after exposure to a number of organisms, including Clostridium difficile, Salmonella, and Campylobacter species. The risk is greater in those taking proton pump inhibitors than with H2 antagonists.
Parasitic
A number of parasites can cause gastroenteritis. Giardia lamblia is most common, but Entamoeba histolytica, Cryptosporidium spp., and other species have also been implicated. As a group, these agents comprise about 10% of cases in children.
Giardia occurs more commonly in the developing world, but this type of illness can occur nearly everywhere. It occurs more commonly in persons who have traveled to areas with high prevalence, children who attend daycare, men who have sex with men, and following disasters.
Transmission
Transmission may occur from drinking contaminated water or when people share personal objects. Water quality typically worsens during the rainy season and outbreaks are more common at this time. In areas with four seasons, infections are more common in the winter. Worldwide, bottle-feeding of babies with improperly sanitized bottles is a significant cause.
Transmission rates are also related to poor hygiene, (especially among children), in crowded households, and in those with poor nutritional status. Adults who have developed immunities might still carry certain organisms without exhibiting symptoms. Thus, adults can become natural reservoirs of certain diseases. While some agents (such as Shigella) only occur in primates, others (such as Giardia) may occur in a wide variety of animals.
Non-infectious
There are a number of non-infectious causes of inflammation of the gastrointestinal tract. Some of the more common include medications (like NSAIDs), certain foods such as lactose (in those who are intolerant), and gluten (in those with celiac disease). Crohn’s disease is also a non-infectious source of (often severe) gastroenteritis. Disease secondary to toxins may also occur.
Some food-related conditions associated with nausea, vomiting, and diarrhea include ciguatera poisoning due to the consumption of contaminated predatory fish, scombroid associated with the consumption of certain types of spoiled fish, tetrodotoxin poisoning from the consumption of pufferfish among others, and botulism typically due to improperly preserved food.
In the United States, rates of emergency department use for noninfectious gastroenteritis dropped 30% from 2006 until 2011. Of the twenty most common conditions seen in the emergency department, rates of noninfectious gastroenteritis had the largest decrease in visits in that time period.
Diagnosis
Gastroenteritis is typically diagnosed clinically, based on a person’s signs and symptoms. Determining the exact cause is usually not needed as it does not alter the management of the condition.
Gastroenteritis is usually diagnosed by the symptoms that it produces, primarily diarrhea. However, if the symptoms are severe or persistent, your doctor may take a stool (feces) sample to identify the cause of gastroenteritis.
Stool samples may be taken during outbreaks of gastroenteritis, such as those occurring on cruise ships and in hospitals and nursing homes, to identify the virus or bacteria that has caused the outbreak. Also, identifying patients with similar histories of food or drink they have recently consumed often helps to determine the source of the outbreak.
However, stool cultures should be performed in those with blood in the stool, those who might have been exposed to food poisoning, and those who have recently traveled to the developing world. It may also be appropriate in children younger than 5, old people, and those with poor immune function.
Diagnostic testing may also be done for surveillance. As hypoglycemia occurs in approximately 10% of infants and young children, measuring serum glucose in this population is recommended. Electrolytes and kidney function should also be checked when there is a concern about severe dehydration.
Dehydration
A determination of whether or not the person has dehydration is an important part of the assessment, with dehydration typically divided into mild (3–5%), moderate (6–9%), and severe (≥10%) cases. In children, the most accurate signs of moderate or severe dehydration are prolonged capillary refill, poor skin turgor, and abnormal breathing. Other useful findings (when used in combination) include sunken eyes, decreased activity, a lack of tears, and a dry mouth. A normal urinary output and oral fluid intake is reassuring. Laboratory testing is of little clinical benefit in determining the degree of dehydration. Thus the use of urine testing or ultrasounds is generally not needed.
Differential diagnosis
Other potential causes of signs and symptoms that mimic those seen in gastroenteritis that needs to be ruled out include appendicitis, volvulus, inflammatory bowel disease, urinary tract infections, and diabetes mellitus.
Pancreatic insufficiency, short bowel syndrome, Whipple’s disease, coeliac disease, and laxative abuse should also be considered. The differential diagnosis can be complicated somewhat if the person exhibits only vomiting or diarrhea (rather than both).
Appendicitis may present with vomiting, abdominal pain, and a small amount of diarrhea in up to 33% of cases. This is in contrast to the large amount of diarrhea that is typical of gastroenteritis. Infections of the lungs or urinary tract in children may also cause vomiting or diarrhea.
Classical diabetic ketoacidosis (DKA) presents with abdominal pain, nausea, and vomiting, but without diarrhea. One study found that 17% of children with DKA were initially diagnosed as having gastroenteritis.
Risk factors
Gastroenteritis occurs all over the world, affecting people of every age, race, and background.
People who may be more susceptible to gastroenteritis include:
- Young children. Children in child care centers or elementary schools may be especially vulnerable because it takes time for a child’s immune system to mature.
- Older adults. Adult immune systems tend to become less efficient later in life. Older adults in nursing homes, in particular, are vulnerable because their immune systems weaken and they live in close contact with others who may pass along germs.
- Schoolchildren, churchgoers or dormitory residents. Anywhere that groups of people come together in close quarters can be an environment for an intestinal infection to get passed.
- Anyone with a weakened immune system. If your resistance to infection is low — for instance, if your immune system is compromised by HIV/AIDS, chemotherapy, or another medical condition — you may be especially at risk.
Each gastrointestinal virus has a season when it’s most active. If you live in the Northern Hemisphere, for instance, you’re more likely to have rotavirus or norovirus infections between October and April.
Prognosis
The prognosis (outlook) for complete recovery is excellent in most people infected with viral and bacterial causes gastroenteritis, as long as the person keeps well hydrated. Because infants, children, pregnant women, and adults that are elderly or immunosuppressed, usually dehydrate faster than healthy adults and sometimes are more difficult to rehydrate orally, their prognosis can range from excellent to poor. Their prognosis depends on how dehydrated they become and how effective are the attempts to rehydrate the patient.
The prognosis for those patients that develop gastroenteritis symptoms as part of a specific disease process (for example, shigellosis) varies from good to poor, depending on the severity of the specific disease process.
Complications
The main complication of viral gastroenteritis is dehydration a severe loss of water and essential salts and minerals. If you’re healthy and drink enough to replace fluids you lose from vomiting and diarrhea, dehydration shouldn’t be a problem.
Most patients who get gastroenteritis have no complications and will completely recover. The major complication for some patients is dehydration; infants, children, the elderly, and immunosuppressed are at higher risk for this complication. In many third-world countries, hydration of infants is difficult at best so there are many infant deaths worldwide due to dehydration caused by gastroenteritis.
Infants, older adults, and people with suppressed immune systems may become severely dehydrated when they lose more fluids than they can replace. Hospitalization might be needed so that lost fluids can be replaced intravenously. Dehydration can be fatal, but rarely.
Treatment
Most people with stomach flu require no formal treatment. The key to a rapid and safe recovery at home (home remedy) is proper hydration. If dehydration occurs, the patient should be evaluated by a doctor. Many health care professionals choose to begin IV fluids, the treatment of choice for rapid rehydration.
Other medications may be prescribed to reduce the symptoms of gastroenteritis. To reduce vomiting, promethazine (Phenergan), prochlorperazine (Compazine), or ondansetron (Zofran) are often used. Some physicians suggest using these agents only as a suppository or rapidly disintegrating tablet on the tongue since patients may vomit the pills up.
Others may prescribe diphenoxylate and atropine (Lomotil) or lopermadine (Imodium) to slow diarrhea while others do not as the drugs may prolong the disease in some individuals. Many doctors recommend no medical treatment for gastroenteritis symptoms as all of the drugs have side effects and if the patient stays well hydrated, the symptoms usually stop soon anyway.
As the gastroenteritis symptoms abate, especially vomiting, doctors may recommend a BRAT diet (bananas, rice, apples, and toast) for a day or two before returning to the patient’s regular diet. Potatoes, lean meat like chicken, and whole grains can help replace nutrients and electrolytes lost with diarrhea.
Patients who have more serious symptoms or other symptoms in addition to gastroenteritis need to be evaluated, diagnosed, and treated by a physician because the patient will likely have a specific disease that will need treatment. The treatment will depend on the cause of the illness (for example, salmonellosis or Clostridium difficult toxin).
Antibiotics and other treatments may not be recommended for some of these diseases so an accurate diagnosis of the disease is important. For Clostridium difficile infected patients, antibiotic sensitivity testing may need to be done to determine the most effective antibiotics to use.
Most people with gastroenteritis recover within several days without the need for medical treatment, as long as they stay properly hydrated. To help keep yourself comfortable and prevent dehydration while you recover, try the following:
- Stop eating solid foods to let your stomach settle
- Avoid dairy products, caffeine, alcohol, nicotine
- Avoid sugary, fatty, or highly seasoned foods
- Drink plenty of liquid every day, taking small, frequent sips, including clear thin broths or soups, diluted non-caffeinated sports drinks (e.g. Powerade or Gatorade), and rehydration formulas (e.g. Gastrolyte) that are available without prescription from a pharmacy
- Ease back into eating slowly with bland easy-to-digest foods such as crackers, toast, bananas, rice, and potatoes
- Make sure that you get plenty of rest
- Avoid taking non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and diclofenac, for pain relief as they can make your stomach more upset
- Paracetamol (e.g. Panadol) can be taken for fever and abdominal pain but it should be used cautiously.
For infants with gastroenteritis, let the baby’s stomach rest for 15 to 20 minutes after vomiting or a bout of diarrhea, then offer small amounts of liquid. Let the baby nurse if being breast-fed. If you are bottle-feeding, offer a small amount of an oral rehydration solution or regular formula.
Anti-diarrhoeal medications, such as Imodium, can be taken to slow the diarrhoea. In most cases, however, it is better for the body to clear itself of the virus or bacteria causing gastroenteritis.
The use of antibiotics is also usually avoided because they are not effective against viruses, and their overuse contributes to the development of antibiotic-resistant strains of bacteria.
When to get medical advice
You don’t normally need to see your GP if you think you have gastroenteritis, as it should get better on its own.
Visiting your GP surgery can put others at risk, so it’s best to phone 111 or your GP if you’re concerned or feel you need advice.
Get medical advice if:
- you have symptoms of severe dehydration, such as persistent dizziness, only passing small amounts of urine or no urine at all, or if you’re losing consciousness
- you have bloody diarrhoea
- you’re vomiting constantly and are unable to keep down any fluids
- you have a fever over 38C (100.4F)
- your symptoms haven’t started to improve after a few days
- in the last few weeks, you’ve returned from a part of the world with poor sanitation
- you have a serious underlying condition, such as kidney disease, inflammatory bowel disease or a weak immune system, and have diarrhoea and vomiting
Your GP may suggest sending off a sample of your poo to a laboratory to check what’s causing your symptoms. Antibiotics may be prescribed if this shows you have a bacterial infection.
Looking after a child with gastroenteritis
You can look after your child at home if they have diarrhoea and vomiting. There’s not usually any specific treatment and your child should start feeling better in a few days.
You don’t normally need to get medical advice unless their symptoms don’t improve or there’s a risk of a more serious problem.
To help ease your child’s symptoms:
- Encourage them to drink plenty of fluids. They need to replace the fluids lost from vomiting and diarrhoea. Water is generally the best. Avoid giving them fizzy drinks or fruit juice, as they can make their diarrhoea worse. Babies should continue to feed as usual, either with breast milk or other milk feeds.
- Make sure they get plenty of rest.
- Let your child eat if they’re eating solids and feel hungry. Try small amounts of plain foods, such as soup, rice, pasta, and bread.
- Give them paracetamol if they have an uncomfortable fever or aches and pains. Young children may find liquid paracetamol easier to swallow than tablets.
- Use special rehydration drinks made from sachets bought from pharmacies if they’re dehydrated. Your GP or pharmacist can advise on how much to give your child. Don’t give them antidiarrhoeal and anti-vomiting medication, unless advised to by your GP or pharmacist.
Make sure you and your child wash your hands regularly while your child is ill and keep them away from school or nursery until at least 48 hours after their symptoms have cleared (see Preventing gastroenteritis).
Getting medical advice for your child
You don’t usually need to see your GP if you think your child has gastroenteritis, as it should get better on its own, and taking them to a GP surgery can put others at risk.
Phone the 111 services or your GP if you’re concerned about your child, or they:
- have symptoms of dehydration, such as passing less urine than normal, being unusually irritable or unresponsive, pale or mottled skin, or cold hands and feet
- have blood in their poo or green vomit
- are vomiting constantly and are unable to keep down any fluids or feeds
- have had diarrhoea for more than a week
- have been vomiting for three days or more
- have signs of a more serious illness, such as a high fever (over 38C or 100.4F), shortness of breath, rapid breathing, a stiff neck, a rash that doesn’t fade when you roll a glass over it, or a bulging fontanelle (the soft spot on a baby’s head)
- have a serious underlying condition, such as inflammatory bowel disease or a weak immune system, and have diarrhoea and vomiting
Your GP may suggest sending off a sample of your child’s poo to a laboratory to confirm what’s causing their symptoms. Antibiotics may be prescribed if this shows they have a bacterial infection.
Prevention
Lifestyle
A supply of easily accessible uncontaminated water and good sanitation practices are important for reducing rates of infection and clinically significant gastroenteritis. Personal measures (such as handwashing with soap) have been found to decrease rates of gastroenteritis in both the developing and developed world by as much as 30%.
Alcohol-based gels may also be effective. Food or drink that is thought to be contaminated should be avoided. Breastfeeding is important, especially in places with poor hygiene, as is the improvement of hygiene generally. Breast milk reduces both the frequency of infections and their duration.
Vaccination
Due to both its effectiveness and safety, in 2009, the World Health Organization recommended that the rotavirus vaccine be offered to all children globally. Two commercial rotavirus vaccines exist and several more are in development.
In Africa and Asia, these vaccines reduced severe disease among infants, and countries that have put in place national immunization programs have seen a decline in the rates and severity of the disease.
This vaccine may also prevent illness in non-vaccinated children by reducing the number of circulating infections. Since 2000, the implementation of a rotavirus vaccination program in the United States has substantially decreased the number of cases of diarrhea by as much as 80 percent.
The first dose of vaccine should be given to infants between 6 and 15 weeks of age. The oral cholera vaccine has been found to be 50–60% effective over 2 years.
The best way to prevent the spread of intestinal infections is to follow these precautions:
- Get your child vaccinated. A vaccine against gastroenteritis caused by the rotavirus is available in some countries, including the United States. Given to children in the first year of life, the vaccine appears to be effective in preventing severe symptoms of this illness.
- Wash your hands thoroughly. And make sure your children do, too. If your children are older, teach them to wash their hands, especially after using the toilet. It’s best to use warm water and soap and to rub hands vigorously for at least 20 seconds, remembering to wash around cuticles, beneath fingernails, and in the creases of the hands. Then rinse thoroughly. Carry sanitizing wipes and hand sanitizer for times when soap and water aren’t available.
- Use separate personal items around your home. Avoid sharing eating utensils, drinking glasses, and plates. Use separate towels in the bathroom.
- Keep your distance. Avoid close contact with anyone who has the virus, if possible.
- Disinfect hard surfaces. If someone in your home has viral gastroenteritis, disinfect hard surfaces, such as counters, faucets, and doorknobs, with a mixture of 2 cups (0.47 liters) of bleach to 1 gallon (3.8 liters) of water.
- Check out your child care center. Make sure the center has separate rooms for changing diapers and preparing or serving food. The room with the diaper-changing table should have a sink as well as a sanitary way to dispose of diapers.
Take precautions when traveling
When you’re traveling in other countries, you can become sick from contaminated food or water. You may be able to reduce your risk by following these tips:
- Drink only well-sealed bottled or carbonated water.
- Avoid ice cubes, because they may be made from contaminated water.
- Use bottled water to brush your teeth.
- Avoid raw food — including peeled fruits, raw vegetables, and salads — that has been touched by human hands.
- Avoid undercooked meat and fish.
The following actions can be taken to avoid getting and spreading gastroenteritis:
- Frequent and thorough hand washing, especially before eating or preparing food, and after going to the toilet or contact with an infected person
- Ensure that children wash their hands frequently and thoroughly
- Avoid direct contact with infected individuals, if possible
- Stay home from work and keep children away from day-care or school until symptoms have gone
- Washing the clothing, bedding, and toys of an infected person
- Cleaning and disinfecting kitchen surfaces, especially after working with raw meat or chicken, or eggs
- Avoid eating undercooked foods, especially meat, chicken, and fish
- Avoid drinking untreated water
- Avoid eating raw meats, fish, and shellfish unless you are sure that they have been freshly prepared and are from a reliable source
- Thoroughly wash any fresh produce, such as fruits and vegetables
- Has your infant or child vaccinated with a rotavirus vaccine, which can prevent gastroenteritis caused by rotavirus?
- Drink only bottled or boiled water and avoid ice cubes when traveling, especially in developing countries.
A vaccine for rotavirus is available free for New Zealand babies. The oral vaccine – Rotarix – is given in two doses (at the 6-week and 3-month immunization visits) to reduce the incidence or severity of rotavirus infection which is a very common cause of gastroenteritis in infants and young children.
When should you call a doctor for the stomach flu (gastroenteritis)?
If gastroenteritis symptoms last more than about five days, increase in severity (fever of 101 F or 38.33 C or higher), or a person develops bloody diarrhea, dehydration, constant abdominal pain, or other symptoms see a physician. The patient may have some gastroenteritis symptoms but may have a disease more serious than self-limiting gastroenteritis.
Signs and symptoms of dehydration may include decreased or no urine production, dry mucus membranes, dry mouth or skin, no tears, weakness, lightheadedness, and low blood pressure, while children may show little or no urination, become lethargic, have skin that “tents up” when pinched. Signs of dehydration in anyone are good reasons to see a doctor immediately.
If you’re an adult, call your doctor if:
- You’re not able to keep liquids down for 24 hours
- You’ve been vomiting for more than two days
- You’re vomiting blood
- You’re dehydrated — signs of dehydration include excessive thirst, dry mouth, deep yellow urine or little or no urine, and severe weakness, dizziness, or lightheadedness
- You notice blood in your bowel movements
- You have a fever above 104 F (40 C)
For infants and children
See your doctor right away if your child:
- Has a fever of 102 F (38.9 C) or higher
- Seems lethargic or very irritable
- Is in a lot of discomfort or pain
- Has bloody diarrhea
- Seems dehydrated — watch for signs of dehydration in sick infants and children by comparing how much they drink and urinate with how much is normal for them
If you have an infant, remember that while spitting up may be an everyday occurrence for your baby, vomiting is not. Babies vomit for a variety of reasons, many of which may require medical attention.
Call your baby’s doctor right away if your baby:
- Has vomiting that lasts more than several hours
- Hasn’t had a wet diaper in six hours
- Has bloody stools or severe diarrhea
- Has a sunken soft spot (fontanel)on the top of his or her head
- Has a dry mouth or cries without tears
- Is unusually sleepy, drowsy or unresponsive
What natural and home remedies are effective against viral gastroenteritis?
In addition to rehydrating and resting, there are some natural and home remedies that may help you feel relief from viral gastroenteritis.
A heating pad or heat pack
Try applying a low-temperature heating pad or a warm heat pack on your stomach to ease cramping. Cover the heating pad with a cloth and don’t leave it on for more than 15 minutes at a time.
Brown rice
Some parents serve rice water for their children. This is the water that remains after boiling brown rice. It’s high in electrolytes and can help to rehydrate much as an OHS can.
Cool the rice water before serving.
Ginger
Products containing ginger, such as ginger ale or ginger tea, can help to soothe an upset stomach.
Mint
Mint may also have anti-nausea properties similar to those of ginger. Sipping a soothing mint tea may help you feel better.
Yogurt or kefir
Although dairy products should be avoided when you have your most acute symptoms, eating unflavored yogurt with live active cultures or drinking kefir may help to restore your body’s natural bacterial balance after an illness.
What’s the long-term outlook?
Viral gastroenteritis generally resolves without medical treatment within two or three days. Most people fully recover with no lasting side effects.
How can you prevent viral gastroenteritis?
- Viral gastroenteritis is easily spread. There are some things you can do to lower your chances of contracting the virus or spreading it to others.
- Wash your hands often, especially after using the bathroom and before food preparation. If necessary, use hand sanitizer until you can access soap and water.
- Don’t share kitchen utensils, plates, or towels if someone in your household is sick.
- Don’t eat raw or undercooked foods.
- Wash fruits and vegetables thoroughly.
- Take special precautions to avoid contaminated water and food when traveling. Avoid ice cubes and use bottled water whenever possible.
- Ask your doctor if you should have your infant vaccinated against rotavirus. There are two vaccines, and they’re generally started around 2 months old.



No Comments