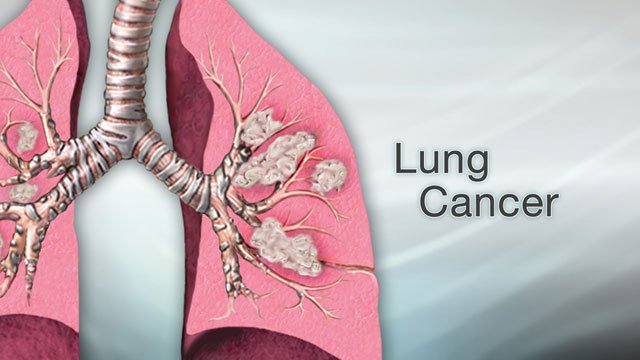
Lung cancer starts in the cells of the lung. A cancerous (malignant) tumour is a group of cancer cells that can grow into and destroy nearby tissue. It can also spread (metastasize) to other parts of the body. When cancer starts in lung cells, it is called primary lung cancer. The lung is part of the respiratory system. You use your lungs when you breathe. The lungs are in the chest, one on each side of the heart.
The right lung has 3 main parts, called lobes. The left lung is a bit smaller and has 2 lobes. The lungs are cushioned and protected by a thin covering called the pleura. For many years, lung cancer was considered a man’s disease. The reality, however, is that lung cancer is the most common cancer-related cause of death among men and women. In 1987, lung cancer surpassed breast cancer to become the leading cause of cancer death among U.S. women.
Cells in the lung sometimes change and no longer grow or behave normally. These changes may lead to non-cancerous (benign) tumours such as hamartoma and papilloma. But in some cases, changes to lung cells can cause cancer.
Lung cancers are divided into non–small cell lung cancer and small cell lung cancer based on the type of cell in which the cancer started.
Non–small cell lung cancer usually starts in glandular cells on the outer part of the lung. This type of cancer is called adenocarcinoma. Non–small cell lung cancer can also start in flat, thin cells called squamous cells. These cells line the bronchi, which are the large airways that branch off from the windpipe (trachea) into the lungs. This type of cancer is called squamous cell carcinoma of the lung. Large cell carcinoma is another type of non–small cell lung cancer, but it is less common. There are also several rare types of non–small cell lung cancer. These include sarcoma and sarcomatoid carcinoma.
Small cell lung cancer usually starts in cells that line the bronchi in the centre of the lungs. The main types of small cell lung cancer are small cell carcinoma and combined small cell carcinoma (mixed tumour with squamous or glandular cells).
Other types of cancer can spread to the lung, but this is not the same disease as primary lung cancer. Cancer that starts in another part of the body and spreads to the lung is called lung metastasis. It is not treated in the same way as primary lung cancer. Find out more about lung metastasis.
A rare type of cancer called pleural mesothelioma is often mistakenly called a lung cancer. But pleural mesothelioma starts in the pleura covering the lung and is very different from cancer that starts in the lung.
In 2012, there will be an estimated 226,160 new cases of lung cancer accounting for about 14 percent of all cancers: an estimated 116,470 cases will be diagnosed in men and 109,690 in women. There will be approximately 160,340 lung cancer deaths (72,590 in women), accounting for 27 percent of all cancer deaths, according to the American Cancer Society. Overall, a woman has a one in 16 chance of developing lung cancer during her lifetime; if she smokes, her chances are much higher.
The incidence of lung cancer in women as a whole has climbed at an alarming rate. And since 1950, the lung cancer mortality rate for American women has increased significantly. These increases are clearly attributable to the increases in the number of women who have smoked.
Lung cancer occurs most often in people over 50 who have a long history of cigarette smoking. Normal lung tissue is made up of cells programmed by genes to create tissue in a certain shape and to perform certain functions. Lung cancer develops when the genetic material responsible for the production of these cells is damaged, or mutates. Repeated exposure to carcinogens, such as tobacco smoke, causes the mutations. This damage is known as genetic mutation.
Mutations in the genetic material of the lung cells cause the instructions for those cells to go awry. Consequently, those cells and their offspring reproduce at a dramatic pace without regard for the normal shape and function of the lung. That wild reproduction causes the formation of tumors that may block air passages in the lung and prevent it from functioning as it should. Mutations may also prevent normal programmed cell death, in which normal cells commit a kind of “suicide.” Because cancer cells are abnormal, this lack of cell death adds to the accumulation of cells and tumor formation.
Some genes are known as tumor suppressors. Their job is to keep abnormal cells from growing and forming tumors. Some women inherit genes from their parents that are more resistant to damage and cancer than others. Those whose genes do not provide as much protection against cancer are said to be genetically susceptible to the disease. Scientists have shown that some cancers (e.g., breast cancer) involve genes that are passed down from parents to their children, and the link between such genetic mutations and lung cancer is also becoming more probable. But the link to heredity has not been absolutely confirmed in lung cancer.
While genetic mutations may play a role, we know that smoking is the number one cause of lung cancer—about 80 percent of lung cancers are thought to be the result of smoking, according to the American Lung Association. Cigarette smoke contains more than 4,000 different chemicals, 60 of which are proven carcinogens, and hundreds of others increase the cancer-causing power of carcinogens.
The more you smoke and the longer you smoke, the greater your risk of lung cancer. But if you stop smoking, the risk decreases steadily each year as abnormal cells are replaced by normal ones. However, the risk never completely returns to the same risk as that of people who never smoked. Since smoking cessation efforts in the United States have been reasonably successful, lung cancer is now very often a disease of former smokers.
The second most common risk factor for lung cancer in the United States is exposure to radon, particularly when combined with cigarette smoking. Radon is a radioactive gas found in the earth’s rocks and soil. It is formed by the natural breakdown of radium, which is a radioactive product of decaying uranium. Radon problems have been identified in almost every state.
This invisible, odorless gas can enter homes from the soil under foundations. Lung cancer risk increases when radon levels are present at high levels in the home and exposure occurs over a long period of time, according to the American Cancer Society. You can measure the radon level in your home with a test kit available in hardware stores. You can also hire a company to come to your home to check radon levels. The testing should be conducted more than once, with the results averaged together.
Another leading cause of lung cancer is on-the-job exposure to carcinogens. Asbestos is perhaps the best-known industrial substance associated with lung cancer, but there are many cancer-causing substances that people may deal with at work. Others include uranium, arsenic and certain petroleum products.
Lung cancer takes years to develop. After exposure to carcinogens, a few unusual cells begin to develop. With continued exposure, more abnormal cells appear. These cells may be on their way to becoming cancerous and forming a tumor.
Lung tumors almost always start in the spongy, pinkish-gray walls of the bronchi—the tubular, branching airways of the lungs. Although there are numerous types of malignant tumors that originate in the lung itself (primary lung cancer), the two major types are small-cell lung cancer and non-small-cell lung cancer.
Non-small-cell lung cancer has three subvarieties:
- Adenocarcinoma accounts for about 40 percent of lung cancers. Adenocarcinoma tends to originate along the outer edges of the lungs in the small bronchi or smaller bronchioles. People with a type of adenocarcinoma called adenocarcinoma in situ(previously called bronchioloalveolar carcinoma) generally have a better outlook than those who have other types of lung cancer. Patients with adenocarcinoma have usually been smokers, but when lung cancer develops in nonsmokers, it is almost always adenocarcinoma type.
- Squamous cell carcinoma accounts for about 25 percent to 30 percent of lung cancers. These tumors are usually found in the middle of the lungs, near a bronchus, and are almost always linked to smoking. Squamous cell carcinoma most often starts in cells of the central bronchi, the largest branches of the bronchial tree.
- Large-cell (undifferentiated) carcinomas are a group of cancers with large, abnormal-looking cells that may appear in any part of the lung.
Small-cell lung cancer comprises about 10 percent to 15 percent of lung cancers and is the most aggressive form of the disease. Like squamous cell carcinoma, this cancer usually originates in the central bronchi. It spreads quickly, often before symptoms appear, making it particularly threatening. It frequently spreads (metastasizes) to the liver, bone and brain. Although usually very responsive to chemotherapy, small-cell lung cancer is less curable than other types because it usually isn’t discovered until it has spread.
The symptoms of lung cancer vary, depending on several factors, including where in the lung the tumor is located. If the cancer is located in one of the bronchi, it can irritate the lining of the bronchus (one of the main airways that branches off of the trachea or windpipe) and cause a chronic cough. The cancerous area may bleed when a person coughs.
If the tumor grows larger, it may gradually fill the bronchus so air can’t pass in or out. A blocked bronchus may cause repeated lung infections or pneumonia.
A tumor in the outer part of the lung may not produce any symptoms until it is fairly large. Sometimes the first sign may be chest pain from the tumor growing into the lining of the lung or the ribs and muscle of the chest wall. If the pleura, or lining of the lung, is involved, it often produces fluid, called a pleural effusion.
This leads to shortness of breath because the fluid prevents the lung from expanding during breathing. Tumors that develop at the very top of the lung may irritate the nerves that supply the arm and cause severe pain or numbness in the arm. This is known as a superior sulcus, or Pancoast, tumor.
A person’s lungs have extensive networks of blood and lymph vessels. Cancer cells may grow into these vessels and be carried by the blood or lymph to circulate through the body. The cancer cells may then be deposited in other organs of the body. A new colony of cancer cells, which starts in another organ, is known as a metastasis.
The first site of tumor metastasis is usually the lymph nodes at the root of the lungs (hilar nodes) and the mediastinum (the space between the two lungs in the middle of the chest). Lymph nodes are small, bean-shaped structures found throughout the body. They produce and store infection-fighting cells.
It is possible for cancer cells that begin in other organs to spread to the lungs. These cases are very different medical problems, however. Depending on the organ of origin, such cases might be termed “primary breast cancer, metastatic to the lungs,” or “primary kidney cancer, metastatic to the lungs.”
Diagnosis
Lung cancer can cause a number of symptoms, including:
- Nagging cough
- Chest, shoulder or back pain, which feels like a constant ache that may or may not be related to coughing
- Shortness of breath
- Fatigue and weakness
- Weight loss
- Repeated episodes of pneumonia or bronchitis
- Coughing up blood
- Hoarseness from left-sided tumors if the nerve that controls the left vocal cord becomes injured by the tumor
- Swelling of the neck, face and arms due to a right-sided tumor compressing the superior vena cava, the main vein that drains the upper body
- Symptoms related to a metastasis, such as headache or weakness from the spread of the tumor to the brain, or back pain related to its spread to the spine.
- Symptoms from paraneoplastic syndromes, disorders caused by a hormonal or an immune response of the body to the presence of the cancer. Examples include certain hormone imbalances, neurologic complications and kidney problems. The symptoms of a paraneoplastic syndrome occur regardless of the location of the tumor or its spread. Sometimes a paraneoplastic syndrome precedes the diagnosis of the cancer and leads to a search for cancer.
A lung cancer may sometimes grow undetected for more than a year without producing symptoms. In fact, lung cancer usually spreads outside the lungs without initially causing any symptoms.
It is difficult to diagnose lung cancer at an early stage. Frequently, people don’t have symptoms, or symptoms are vague or attributed to other ailments, such as stress, bronchitis, pulled muscles or pneumonia.
When lung cancer is suspected, a series of tests are conducted to confirm the disease and to determine how widely the cancer has spread (staging).
The major tests include:
X-rays:
A chest X-ray is frequently ordered as a first step in diagnosis. An X-ray is a two-dimensional picture that can help locate a tumor. If nothing shows up on the X-ray, you probably don’t have lung cancer. If your health care professional sees something suspicious, he or she may order additional tests.
Computed tomography imaging (CT scan) or magnetic resonance imaging (MRI):
These tests may help your health care professional confirm a diagnosis suspected from a chest X-ray. CT scans and MRIs use computerized pictures to show very detailed three-dimensional and cross-sectional images of the body. They can depict the size, shape and location of a tumor.
These tools are also used to find out if the tumor has spread from the lung to lymph nodes or other organs in the chest or to other parts of the body.In recent years a type of CT scan called spiral CT has become increasingly more available in medical centers across the country.
Spiral CT uses a faster machine that rotates continuously around the body, allowing it to more quickly detect images and identify abnormalities. It can also detect small nodules (early-stage disease) that are not very visible on chest X-rays. Another advantage of spiral CT is that it delivers a lower dose of radiation than traditional CT scans.
The disadvantages of spiral CT scans are that they are expensive, and they often find tiny nodules that are not cancerous; in that case, additional testing or even major surgery are required to prove they are benign. Spiral CTs also can be used to look for masses in the adrenal glands, brain and other internal organs that may be affected if lung cancer has spread.
Positron emission tomography (PET):
In this procedure, the patient is injected intravenously with a small amount of radioactive sugar that cancer cells absorb, enabling the cells to be seen by a special camera. It is based on the premise that cancerous tissue utilizes more sugar than normal tissue, leading cancers to “light up” on the PET scan. The technique is very sensitive and even very small malignant tumors can show up easily.
The test is used to determine if the cancer has spread to lymph nodes or other distant places. It is also used to tell if a shadow on your chest X-ray is cancer. Most insurance companies cover expenses for PET imaging, including Medicare. Both false-positive and false-negative PET findings may occur, however (in which the scan shows what looks like cancer, but really isn’t, or doesn’t show the cancer when it really exists), so it’s important that the scans be interpreted very carefully.
In addition, there are newer machines available that can perform a PET and CT scan at the same time (PET/CT scan). With this test, health care professionals can compare areas of higher radioactivity on the PET scan with the appearance of the same areas on the CT scan for clearer localization of abnormalities and clarification of uncertain findings.
- Bone scan: A bone scan can help determine whether or not lung cancer has spread to the bones. During this test, a small amount of radioactive dye is injected into a vein. It accumulates in areas of bone that may be cancerous. Then a gamma camera scans your body to detect where bone repair is occurring faster than the surrounding bone. This is a sign that the cancer has infiltrated and is destroying the bone.
- Needle biopsy is just like it sounds: a needle is inserted through the chest wall to take a sample of tissue from a known tumor after it’s been located by chest X-ray, CT scan or fluoroscopy (fluoroscopy is like an X-ray, but the image is viewed on a screen in real time rather than on film). The sample is then examined under a microscope to see if cancer cells are present. A biopsy is necessary for your health care professional to confirm a cancer diagnosis and to identify the specific type of cancer and its stage. Sometimes a needle biopsy will be done of an area that is suspicious for a metastasis, such as the liver or adrenal gland, to prove that a metastasis is present.
- Surgical biopsy is a test in which the chest wall is opened to remove part or all of the tumor. A pathologist examines tissue samples and provides information about the type of cancer present and the stage of the cancer.
- Bronchoscopy is a procedure in which a flexible lighted tube (bronchoscope) is inserted through the nose or mouth and into the airways to collect bronchial and/or lung secretions or to biopsy for tissue specimens. To make the procedure more comfortable, your mouth and throat may be sprayed first with a numbing medicine, or you may be given medication to make you feel more relaxed.
- Mediastinoscopy is a procedure in which a surgeon makes a small cut in your neck and inserts a hollow lighted tube behind the sternum (breast bone), while you’re under general anesthesia. The surgeon then uses the tube to guide instruments into the chest to sample tissue from the mediastinal lymph nodes along the windpipe and major bronchial tube areas. The samples are evaluated under a microscope.
- Mediastinotomy is a surgical procedure that opens the chest cavity to remove samples of mediastinal lymph nodes while you’re under general anesthesia. More lymph nodes can be sampled in this way than with the mediastinoscopy procedure, particularly those on the left side.
- Thoracentesis is a procedure in which the doctor places a needle between your ribs to drain accumulated fluid around the lungs (called pleural effusion) and examines it microscopically for the presence of cancer cells. Malignant pleural fluid can indicate that cancer has spread to the delicate membranes that cover the lungs (called pleural membranes). Fluid accumulation can also prevent the lungs from filling with air, so thoracentesis can improve your breathing.
- Thoracoscopy is a procedure in which the surgeon uses a thin, lighted tube connected to a video camera and monitor to view the space between the lungs and chest wall and remove small pieces of tissue for examination under a microscope. It is commonly called VATS (video-assisted thoracic surgery). Like thoracentesis, this examination checks whether a pleural effusion is the result of cancer metastasis to the pleural membranes or related to some other condition such as heart failure or an infection.
- Blood counts and blood chemistry tests are not used alone to diagnose lung cancer, but they can spot abnormalities in some of your organs that may signal cancer and may be used to determine whether or not you are healthy enough to undergo surgery. If cancer has spread to the liver and bones, for instance, it may cause certain chemical abnormalities in the blood. If one of these abnormalities in particular, called the LDH, is significantly elevated, it usually means that the outlook for cure or long-term survival isn’t good. A complete blood count (CBC) may also be performed and repeated regularly if you are being treated with chemotherapy to make sure you’re not becoming anemic as a result of the treatment and that your white blood cells and platelets are sufficiently high to permit continued therapy.
The stages of non-small-cell cancer are:
- Occult stage: Cancer cells are found in sputum (mucus) or other lung fluids, but no tumor can be found on x-rays.
- Stage 0: Cancer is only found in a local area and only in a few layers of cells. It has not grown through the top lining of the lung or spread to lymph nodes or distant sites. Another term for this type of lung cancer is carcinoma in situ.
- Stage I: The cancer has not invaded the lymph nodes or area outside the chest.
- Stage II: The cancer has spread to nearby lymph nodes or invaded the chest wall.
- Stage III: The cancer has spread to the lymph nodes in the area that separates the two lungs (mediastinum); or to the lymph nodes on the other side of the chest or in the lower neck.
- Stage IV: Cancer has spread to other parts of the body.
- Recurrent: Cancer has come back (recurred) after previous treatment.
There are a number of ways health care professionals stage small-cell lung cancer, with the simplest method being the following:
- Limited stage: Cancer is found only in one lung and in nearby lymph nodes.
- Extensive stage: Cancer has spread outside of the lung to other tissues in the chest or other parts of the body.
Recurrent disease means that the cancer has come back (recurred) after it has been treated. It may come back in the lungs or in another part of the body.
Treatment
The three primary forms of treatment for lung cancer are surgery, radiation therapy and chemotherapy. One or more of these therapies may be used to treat lung cancer, depending on the type and stage of the disease as well as your age and overall health. When you’re considering treatment options, it’s a good idea to seek a second opinion to get more information and help you feel more confident about your chosen treatment plan.
Surgery
Surgery is primarily used to remove the cancerous tumor from the lung. This therapy, called surgical resection, is typically used when the cancer has not spread to other tissues in the chest or elsewhere in the body. It may be the first type of treatment you receive or it may follow chemotherapy and/or radiation, which are sometimes used first to shrink the tumor(s).
During the procedure, a surgeon usually removes nearby lymph nodes to check them for cancer. A widespread misconception is that lung surgery exposes tumors to the air, which makes them spread. This is absolutely false. If the cancer does spread, the growth occurred microscopically before the cancer was diagnosed and before surgery was ever performed.
Three types of surgery are used in the treatment of lung cancer:
- Wedge or segmental resection: If the tumor is small enough, a surgeon may be able to treat it by removing the part of the lung that is affected. This type of surgery may also be used in patients whose lung function does not allow for more lung tissue to be removed.
- Lobectomy: An entire section (lobe) of the lung is removed. This is the most common operation performed for lung cancer.
- Pneumonectomy: Removal of the entire lung.
There are cases where initial surgery is not recommended. (Other types of surgery still may be used to relieve symptoms, however.)
For example, when:
- Cancer has spread to the other lung;
- Cancer has grown from the lung into mediastinal lymph nodes or other organs in the chest;
- Cancer has spread to the lymph nodes in the neck or to other organs, such as the liver, bones or brain;
- There are other health-related problems that make major surgery unsafe.
More recently, a less invasive surgical procedure for treating early stage lung cancer—called video-assisted thoracoscopic surgery—has been developed. This procedure involves the insertion of a small hollow tube with a video camera attached to the end into the chest to help the surgeon see the tumor.
Only small incisions are needed to make room for the tube, so there is less pain and a shorter recovery period than with standard surgery. However, most experts recommend the procedure only be used for tumors smaller than three to four centimeters (about an inch and a half). Also, because this surgery requires more technical skill than the standard procedure, it is important that it be done by a specially trained and experienced surgeon.
After surgery, you may experience significant pain, and you should receive pain medication to control it. Some pain, however, is tenacious. Many people who have lung surgery complain of lasting pain at the incision sites. This is especially difficult for women because the incision line is often right at the bra line. Many women find alternatives to tight clothing to avoid this irritating and lasting pain. In some instances, nerve blocks performed by an anesthesiologist may help this problem.
Radiation therapy
Many women with lung cancer will need radiation therapy at some time during their illness, either as a primary treatment or as a means of symptom management called palliation. Radiation therapy consists of directing a beam of high-energy rays at a tumor. By injuring cancer cells so they can’t continue to multiply, the radiation slows or stops tumor growth. The amount of radiation used is based on the size and location of the tumor.
Another form of radiation, called brachytherapy, involves placing a small pellet of radioactive material through a bronchoscope right into the tumor or the airway closest to the cancer. Side effects associated with radiation include fatigue, dry or sore throat, skin irritation and loss of hair in the treated area. In patients with stage III non-small-cell lung cancer, radiation is a key part of the therapy, usually combined with chemotherapy. Remissions are common, and long-term remissions may occur in some patients.
Chemotherapy
Anticancer drugs are taken intravenously or, sometimes, orally. They circulate throughout the bloodstream killing fast-growing cells like cancer cells. Chemotherapy can be used to destroy the cancer, slow its growth, keep it from spreading or relieve symptoms. Even if chemotherapy doesn’t get rid of all the cancer, studies find it can help lung cancer patients live longer and more comfortable lives.
Chemotherapy is usually administered in an outpatient setting and in regular intervals (cycles) at regular doses for several months. In most cases, cycles last three to four weeks, and initial treatment usually consists of four to six cycles. A wide variety of chemotherapy drugs are used for the treatment of lung cancer, and sometimes, two different chemotherapy drugs are given at the same time. For non-small-cell lung cancer, the most common combinations include the use of carboplatin (Paraplatin) or cisplatin (Platinol), in combination with a second drug.
Other commonly used drugs are docetaxel (Taxotere), paclitaxel (Taxol), vinorelbine (Navelbine), gemcitabine (Gemzar), irinotecan (Camptosar), etoposide (VePesid,), vinblastine (Velban) and pemetrexed (Alimta).
Combining cisplatin or carboplatin with other agents such as gemcitabine and paclitaxel appears to be more effective than using one drug alone to treat non-small-cell lung cancer. However, single-drug chemotherapy may be used for people with non-small-cell lung cancer who might not tolerate combination chemotherapy well, such as those in poor general health.
Studies have shown that combinations of two chemotherapy drugs are as effective as combinations of three, and that two-drug combinations produce fewer side effects.
If non-small-cell lung cancer relapses, the drugs typically used for therapy are docetaxel (Taxotere), pemetrexed (Alimta) and erlotinib (Tarceva).
Patients with small-cell lung cancer usually initially receive a combination of two to three chemotherapy drugs.
The most common combinations are:
- cisplatin (Platinol) and etoposide (VePesid)
- carboplatin (Paraplatin) and etoposide (VePesid)
- cisplatin (Platinol) and irinotecan (Camptosar)
- carboplatin (Paraplatin) and irinotecan (Camptosar)
- cyclophosphamide (Cytoxan), doxorubicin (Adriamycin) and vincristine (Oncovin)
If the cancer progresses during treatment or returns after treatment, your health care professional may try different chemotherapy drugs depending in part on how soon the cancer begins to grow again. If the cancer progresses during treatment or relapses within two to three months of when the initial treatment ended, your health care professional may try topotecan (Hycamtin), paclitaxel (Taxol), docetaxel (Taxotere), irinotecan (Camptosar) or gemcitabine (Gemzar).
If the cancer relapses from two to six months after treatment, your health care professional may try topotecan, irinotecan, cyclophosphamide/doxorubicin/vincristine (known as the CAV regimen), gemcitabine, paclitaxel, docetaxel, oral etoposide or vinorelbine.
If the cancer relapses six months or more after treatment, your health care professional may try the original chemotherapy regimen again.
Because they reach all the parts of your body, chemotherapy drugs also affect normal cells. Side effects vary greatly. The most common include nausea and vomiting, hair loss, fatigue, susceptibility to infection and constipation. Your health care professional can help you manage these side effects, but you must be sure to communicate how you feel.
Targeted therapy
Newer biologic drugs designed to specifically target and interfere with some aspect of tumor cell function are also used to treat lung cancer. Two, erlotinib (Tarceva) and cetuximab (Erbitux), prevent the production of epidermal growth factor receptor (EGFR), a protein that helps tumor cells grow. Erlotinib has been shown to help keep some lung cancer tumors under control, particularly in women and people who have never smoked.
It is most frequently used for advanced lung cancers and lung cancers that have not responded to chemotherapy. Erlotinib is taken in pill form and may cause a few side effects, the most common being diarrhea, an acne-like rash on the face and chest, loss of appetite and fatigue.
Cetuximab works similarly to erlotinib but is administered intravenously, usually once a week. Some health care professionals may add cetuximab to standard chemotherapy. Side effects are similar to those with erlotinib, but cetuximab may also cause a serious allergic reaction during the first infusion that may lead to breathing problems and low blood pressure. You may be given a medication before you receive cetuximab to prevent this reaction.
A new drug, crizotinib (Xalkori), is an oral targeted drug for the small minority of patients whose tumors express the ALK rearrangement. These are mostly patients who have adenocarcinomas and a minimal smoking history. If that marker is present, crizotinib has a high rate of treatment benefit.
A second type of targeted therapy drug, bevacizumab (Avastin), targets a protein that helps new blood vessels form called vascular endothelial growth factor (VEGF). When added to standard chemotherapy regimens, bevacizumab has been shown to prolong the lives of patients with advanced lung cancer. It is commonly given along with carboplatin plus paclitaxel, where it has been shown to prolong remission longer thanachieved with the chemotherapy drugs alone.
Patients taking bevacizumab get it intravenously every two to three weeks. Bevacizumab can cause bleeding, so it is not usually used in patients who have cancer that has spread to the brain, who are coughing up blood or who are on blood thinners such as warfarin (Coumadin). It can also cause blood clotting problems such as strokes. Bevacizumab is also not usually recommended for people with squamous cell cancer.
Because of the increasing development and availability of targeted drugs, it is becoming more common to test tumor tissue for the presence of the markers that would predict responsiveness to those targeted drugs, for example, EGFR mutations predicting response to erlotinib or ALK rearrangement predicting response to crizotinib. Sometimes that requires obtaining additional tumor tissue biopsies to have sufficient material to test.
Prevention
Unlike many other cancers, there are some steps you can take to prevent lung cancer. If you are a smoker, stop. Numerous smoking cessation courses and aids are available today. Talk to your doctor about options you can explore. If you are a nonsmoker, try to avoid second-hand smoke. Other preventive steps include:
- Test your home for radon, especially if you live in an area known to have high levels. State radon offices can offer more information on correcting this problem.
- Be aware of and limit exposure to industrial agents at work such as nickel, chromate, asbestos and vinyl chloride.
Facts to Know
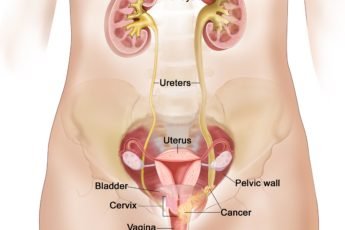
- Cigarette smoking is responsible for about 80 percent of lung cancers among women. Women who smoke are also at increased risk for cancers of the oral cavity, pharynx, larynx, esophagus, pancreas, kidney, bladder and cervix.
- In 2012, there will be an estimated 226,160 new cases of lung cancer, accounting for about 14 percent of all cancers: 116,470 will be diagnosed in men and 109,690 in women, according to the American Cancer Society.
- About 160,340 people will die from lung cancer in 2012, including 72,590 women.
- Since 1950, lung cancer mortality rates for U.S. women have increased significantly. Women still have lower rates of lung cancer than men, but the gap is closing. In 1987, lung cancer surpassed breast cancer to become the leading cause of cancer death among U.S. women.
- There are two major types of lung cancer—small-cell and non-small-cell. Small-cell lung cancer is the more aggressive but less common form, though overall survival rates are similar for both types.
- Persistent cough, sputum streaked with blood, chest pain and recurring pneumonia or bronchitis may sometimes be signs of lung cancer.
- Other risk factors for developing lung cancer include exposure to certain industrial substances, such as arsenic, some organic chemicals, radon and asbestos (particularly for people who smoke); radiation exposure from occupational, medical and environmental sources; air pollution; and second-hand tobacco smoke.
- If a woman stops smoking before cancer develops, damaged lung tissue gradually starts to return to normal.
- Surgery, radiation therapy and chemotherapy are the primary forms of treatment for lung cancer. One or more of these therapies may be used, depending on the type and stage of the disease as well as your age and overall health.
- The five-year relative survival rate for lung cancer depends on the stage the cancer is at when it is found. The survival rate is 45 percent to 49 percent for cases detected when the disease is still localized (stage I), but only a small percentage of lung cancers are discovered that early.
Key Q&A
- What causes lung cancer?Cigarette smoking is responsible for about 80 percent of lung cancers among women.. Another leading cause of lung cancer is on-the-job exposure to carcinogens. Asbestos is perhaps the best known of the industrial substances associated with lung cancer, but there are many cancer-causing substances that people may deal with at work. Some others are uranium, arsenic and certain petroleum products.
- Who usually gets lung cancer?Lung cancer occurs most often in people over 50 who have long histories of cigarette smoking. The incidence of lung cancer in women as a whole has climbed at an alarming rate, and these increases are clearly attributable to the increases in the number of women who have smoked.
- Would a chest X-ray earlier have found lung cancer sooner?Chest X-rays are not recommended as a screening tool. A chest X-ray may have discovered it earlier, but not likely at an earlier stage of cancer, so it likely would not have changed the overall outcome.
- I have lung cancer and my health care professional wants to do a surgical resection (removal of the tumor). How do I know if this is the right thing to do?Do not submit to any procedure until you are clear and have all the answers to your questions. Be aware, however, that if surgery is being considered for lung cancer, it is a good sign, signifying that the degree of tumor involvement or spread is probably limited. Also, you should consider getting a second opinion. Your health care professional should not be offended by this suggestion and, in fact, might encourage it. He or she should conduct a pulmonary function test before surgery; this test helps identify patients with extremely high surgical risk. Also, cardiopulmonary exercise testing may be helpful to determine whether or not you can withstand the rigors of this surgery.
- Does the rest of my family need to be screened for lung cancer?Generally, researchers don’t think of lung cancer as hereditary. There may be a genetic link, but the role of heredity in lung cancer is less well understood than it is for many cancers. There won’t be a genetic test until researchers find a specific genetic link. However, you are considered at an increased risk for lung cancer if you have a close relative with lung cancer, so discuss the matter with your health care professional.
- I’ve heard a lot about environmental tobacco smoke. What is it and what effect does it have on me?More simply put, it’s second-hand smoke. Environmental tobacco smoke (ETS) is the combination of two forms of smoke from burning tobacco products: sidestream smoke, or smoke that is emitted between the puffs of a burning cigarette, pipe or cigar; and mainstream smoke, or the smoke that is exhaled by the smoker. When a cigarette is smoked, about one-half of the smoke generated is sidestream smoke. This form of smoke contains essentially all of the same carcinogenic agents that have been identified in the mainstream smoke, but at greater levels. Researchers estimate that ETS causes about 3,000 lung cancer deaths among nonsmokers each year.
- What can I do to help myself through lung cancer treatment?First, stay active. You may need periods of rest, but there’s no need to stop doing the things you enjoy as long as you feel able to do them. Seeing other people and maintaining a social life is important. In general, anything you feel well enough to do is all right. This includes light activities (like housework or walking), sports and an active sexual life. You may be able to continue working full- or part-time. If you cannot work, it is important to stay involved in as many other activities as possible.
- I’m experiencing severe pain, but I’m afraid that I’ll become addicted if I take heavy-duty drugs. What should I do?First, talk to your health care professional. Don’t accept pain because you have cancer. It can be managed with help from knowledgeable health care professionals. Many myths about pain still exist. The most troubling one is that too much medication will cause addiction. Studies have shown this to be completely false. Addiction is a psychological or emotional dependence on feeling high. People with cancer do not take drugs to get high, but to relieve their pain. When the proper dosage of medication is taken around the clock, addiction does not occur, and if the pain is relieved by surgery or other treatments, continued use of the pain medications is not necessary. Physical tolerance may develop if you take narcotic medications for a long time,, so stopping the medication abruptly may cause you to feel ill for a few days. Tapering the dose over a week or two may be better tolerated, but addiction is not a serious concern in cancer patients.
- I have no appetite from the cancer and the chemotherapy. Everything I put down comes up, so what’s the use of eating?You must eat as much as you can while you are having treatment. People who eat well and drink lots of fluids can deal with side effects better and are better able to fight infection. In addition, their bodies can rebuild healthy tissues faster. Even when you know it’s important to eat well, there may be days when you feel you just can’t. You may be interested to know that cancer generally decreases appetite. Chemotherapy also affects your appetite because it affects how your food tastes, and simply having lung cancer can also wipe out your appetite. When your appetite is poor, try these strategies:
- Eat small meals or snacks whenever you want. You don’t have to eat three regular meals each day. A variety of high-calorie liquid supplements are available, both in creamy and fruit-flavored forms, that may permit good nutritional intake without a high volume of food.
- Vary your diet and try new foods and recipes. Some patients find that cold foods are easier to tolerate because the smell of cooking foods may be a turnoff.
- When possible, take a walk before meals to make you feel hungrier.
- Try changing your mealtime routine. For example, eat by candlelight or in a different location.
- Eat with friends or family members. When eating alone, listen to the radio or watch TV.
- If you live alone, you might want to arrange for Meals on Wheels or a similar program to bring food to you.
- Drink as much as you can. Small amounts consumed often will help keep enough fluids in your body. You may find popsicles, gelatins and ice cream to be good substitutes for other liquids.
- I am so depressed about having lung cancer that I feel I cannot go on.You need help dealing with your feelings. You should immediately seek help from a counselor, therapist, social worker or clergy member. Ask your health care professional what services are available. It may also help to join a support group of people who are living with cancer. Talking with other people who understand and can relate to many of the same issues you are coping with can be a great help.
For more information visit us our website: https://www.healthinfi.com
0 200


No Comments