If you’re feeling confused about mammograms and what type of schedule to stick to, you’re not alone. It seems that every time new guidelines come out, little time passes before those guidelines change once again. And it’s not uncommon to find differing opinions from different organizations, which only makes the issue that much more bewildering. The latest shift comes from the American Cancer Society (ACS).
Why can’t everyone be on the same page?
One reason guidelines change is that concerns are growing about “overdiagnosis,” meaning that there are cancerous tumors that may show up in a mammogram that prove to never present a threat during a woman’s lifetime. As a result, women may go through unnecessary treatment for breast cancer. (A 2012 study published by the New England Journal of Medicine found that an estimated 1.3 million American women had breast cancers that would never have led to clinical symptoms.)
Another reason? There is potential harm in false-positive tests, leading to worry, anxiety and unnecessary breast biopsies.
According to Breastcancer.org, for each breast cancer death that is prevented, three to four women are over-diagnosed. That organization notes that false positives, while good news, can and do result in many extra tests, procedures, doctor visits, and follow-ups. With all the various and varying opinions out there, it’s easy to see why women are confused and unsure about how to best screen for breast cancer. To be prepared and armed to make the best choices and understand the reasoning behind them, we need to understand what’s being said.
Four of five doctors still recommend annual mammograms for women in their early 40s, despite guideline changes that have pushed back the age for yearly breast cancer screening, a new survey shows. Overall, 81 percent of physicians surveyed said they suggest annual mammograms for women aged 40 to 44, while more than two-thirds recommend regular mammograms for women aged 75 or older.
“Gynecologists were, in general, more likely to recommend routine mammograms,” added lead researcher Dr. Archana Radhakrishnan, an internist with Johns Hopkins University in Baltimore. These practices run counter to guidelines issued by the American Cancer Society, which recommends annual screening starting at 45 and screening every other year from age 55 onward, researchers said in background notes.
The doctors also are ignoring the advice of the U.S. Preventive Services Task Force (USPSTF), a volunteer body that helps set standards for preventive care. The USPSTF recommends that women aged 50 to 74 receive mammograms every other year. According to Dr. Deborah Grady, “It’s kind of disappointing and dispiriting to find that such a large proportion of physicians still say they don’t follow the guidelines.” Grady is a professor of epidemiology with the University of California, San Francisco, School of Medicine. She wrote an editorial that accompanied the study, which was published online April 10 in JAMA Internal Medicine.
Mammography recommendations were changed in recent years based on evidence that breast cancer occurs so much less often in women in their 40s that the risks of screening outweigh the benefits, Grady explained. Younger women also have a higher risk of receiving a false positive on a mammogram, which opens them up to more follow-up procedures.
“The false positive may result in some anxiety for the patient, but it definitely will result in additional testing,” Grady said. Women could be exposed to additional radiation during follow-up scans, or have to undergo a biopsy. There’s also a greater risk of overdiagnosis in these women, Grady said — essentially finding cancer that poses no immediate health risk but now must be addressed with lumpectomy, radiation therapy and possible hormone therapy.
Women in their 40s at average risk for breast cancer should talk to their health care provider about the risks and benefits of mammography before starting regular screening at that age, according to guidelines released Thursday by the American College of Obstetricians and Gynecologists. The group had previously recommended annual mammograms starting at age 40. But the advice has changed to better incorporate input from the woman being screened, says physician Christopher Zahn, vice president of practice activities at ACOG. “A patient’s preferences and values need to be an important part” of the decision, he says.
Now the group says providers should offer the test when a woman enters her 40s, and that after a discussion, she may opt to start screening. If she doesn’t, she should start by age 50, ACOG says. Zahn says the guidance intentionally encompasses advice from other major groups.
The U.S. Preventive Services Task Force says women should start regular mammograms at 50, and that women in their 40s should make an individual decision about whether or not to screen. The American Cancer Society says screening should be offered starting at age 40, and outright recommends starting at 45. And the National Comprehensive Cancer Network, an alliance of major cancer centers, recommends starting at 40.
The question all these groups have wrestled with is how to balance the benefits and harms of mammography; their different recommendations reflect differences in how they interpreted and weighed the available data. “All three [schedules] are reasonable approaches to take,” says Zahn.
Mammography clearly saves lives for women over 50 and likely does so overall for women in their 40s, says Otis Brawley, chief medical officer at the American Cancer Society. But the benefits in those younger women are smaller, and they come at the cost of false alarms, unnecessary biopsies and overdiagnosis, when cancer that is detected and treated never would have threatened a woman’s health had it gone undiscovered. (The ACS says estimates of overdiagnosis vary widely, from 0 percent to 54 percent of breast cancers, in part depending on whether cases of ductal carcinoma in situ abnormal cells that sometimes turn into cancer are included.)
Once a woman starts mammography, she can be screened every one or two years, again after a discussion about the pros and cons of the different schedules, ACOG advises. The American Cancer Society recommends annual screening for women through age 54 and every other year for older women, with the option to continue annual tests, while USPSTF says every other year is sufficient and the network of cancer centers recommends annual screening.
A statistical model from the USPSTF finds that if 1,000 women are screened every other year from age 40 to 74, there will be eight fewer breast cancer deaths compared with no screening, 213 unnecessary breast biopsies and 21 over diagnosed breast tumors. Meantime, if 1,000 women are screened every other year from 50 to 74, there will be seven fewer breast cancer deaths compared with no screening, 146 unnecessary biopsies and 19 over diagnosed tumors.
Some women may decide that the small additional benefit doesn’t outweigh the increased risk of biopsy or possibly being treated for a cancer that didn’t need attention. There’s as yet no sure way to know which tumors are harmless and can be left alone. Others may choose differently. “There’s more of a respect for the individual person,” says Brawley about the new ACOG guidelines and the 2015 changes by his own organization. “You’re starting to hear, ‘Let the woman decide.’ “
“If a woman is told to get a mammogram starting at 40, it’s very reasonable to question that and ask, ‘Why? I’ve read that there are conflicting guidelines,’ “says Deanna Attai, assistant clinical professor of surgery at the David Geffen School of Medicine at UCLA.
She says women should know, or ask about, the risk factors for breast cancer so they can have the screening conversation with some understanding of where they fall on the spectrum. And don’t stop the risk-reduction discussion at screening. “Ask what lifestyle or health habits can help reduce risk,” she says. (For example, research suggests exercise can cut breast cancer risk.)
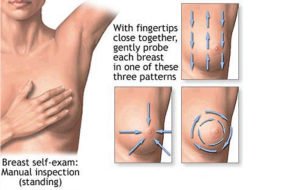
On the question of when to stop routine mammograms, ACOG says screening beyond age 75 should be based on a conversation about a woman’s health status and longevity. The group also recommends against regular breast self-exams but says women should be aware of the normal feel and appearance of their breasts so they can report any changes.
Keep in mind that these recommendations are for average-risk women who are not experiencing symptoms. Many factors can increase risk, including a family history of breast or ovarian cancer and certain genetic mutations. So those women should check with their physician about when, how and how frequently they should be screened. There’s also not enough evidence to make recommendations on whether women with dense breasts should be screened differently.
The ACS says its guidelines were due for an update the group’s most recent recommendations date back to 2003, when it recommended annual mammograms beginning at age 40. “In 2003 nobody talked about the balance of benefits and harms which is now a really a standard for guidelines,” says Dr. Richard Wender, the chief of cancer control at ACS.
This may help clear up at least some of the confusion around when women should start screening, and how frequently they should go in once they start. In 2009, when the U.S. Preventive Services Task Force (USPSTF) said there was insufficient evidence to support the recommendation that women start screening at 40, USPSTF changed its official advice to biennial screening beginning at age 50 for most women. Earlier in 2015, its draft guidelines reinforced the 2009 recommendations. The ACS, meanwhile, continued to recommend a starting age of 40.
“What I can confidently state is that the simple [2003] guideline fueled confusion. It caused women and clinicians to choose, ‘Well, I either follow this guideline or I follow that guideline and I don’t understand why they are so different,'” says Wender. “We know that we have an obligation to make sure that clinicians are educated and the public has the right education and guidance, including more helpful decision making tools.”
The new guidelines are a little more in line with those issued by the USPSTF. ” There are many similarities,” the USPSTF said in a statement about the new ACS guidelines. “We both found that the benefit of mammography increases with age, with women in their 50s, 60s, and early 70s benefiting most from regular mammography screening.”
The new ACS guidelines are more granular than previous ones, with screening advice and frequency broken down by age. “The evidence simply no longer supports one-size-fits-all,” says Dr. Kevin Oeffinger , chair of the ACS breast cancer guideline panel and a family physician at Memorial Sloan Kettering Cancer Center . “In medicine we are moving closer and closer to bringing about a personalized approach.”
In a preemptive response to the new guidelines, the American College of Radiology, which represents doctors and groups that perform mammography, and Society of Breast Imaging, a proponent of early detection, said in a statement release to the media that they “continue to recommend that women get yearly mammograms starting at age 40.”
When asked whether, as a clinician, his own views on screening have changed through the years, Wender said yes. “It’s easy to say that any test that might result in a prevention of a death should be worthwhile, and why wouldn’t you do that for everyone?” he says. “I’ve come to appreciate two things over time. There just is no perfect screening test. And I really have come to embrace a balance of the benefits and drawbacks to screening.”
One of those drawbacks is false positives; over 10 years, a woman getting an annual mammogram has a 61% chance of getting such results. Another is the mounting data that mammograms do not save nearly as many lives as experts hoped they would, and can lead to aggressive treatment of early-stage cancers that may be unnecessary.
The ACS says it recommends all women become familiar with the potential benefits, limitations and harms that come with breast cancer screening. “I continue to impressed with the savviness of American women with regard to health issues,” says Oeffinger. “This is a topic women have spent much time thinking and reading about. We really emphasize the doctor-patient relationship and the opportunity for someone who really knows a patient to answer questions and help them understand the different information out there, and reach a decision together.”
Wender adds: “Although it’s tempting to impose our own values, patients both men and women—want and are able to, with appropriate guidance, make a personal decision.”
What the ACS Now Says
- Published in the Journal of the American Medical Association’s October 2015 issue, the updated breast cancer screening guidelines recommend that women at average risk for breast cancer begin having regular yearly mammograms at age 45. (Its prior recommendation was age 40.)
- Once they reach 55, screening should be scheduled every other year.
How can women deal with the confusion and uncertainty about what recommendations they should follow? A few more recommendations from the ACS that might help clarify the question:
- Become familiar with the potential benefits, harms and limitations that come with breast cancer screening.
- Know that you do have the opportunity to begin annual screening earlier.
- Continue screening as long as your overall health is good and you have a life expectancy of 10 years or more.
- Women at average risk, of any age, are not recommended to get clinical breast exams.
What the U.S. Preventive Services Task Force Says
The U.S. Preventive Services Task Force’s (USPSTF) goal is “empower women with the data so they can make the best health care decisions for themselves.” In April of 2015, this group, whose members gather and review expert opinions and review the science from various specialists including surgeons, oncologists and radiologists, issued new recommendations on breast cancer screening.
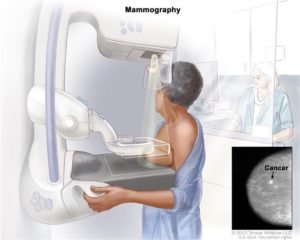
While mammography, whose benefit increases with age, is indeed recognized as an important test in reducing deaths from breast cancer, the information gathered led the USPSTF to recommend screening to be most beneficial for women between the ages of 50 and 74.
Women aged 40 to 49 were recommended to reach a decision that is most comfortable for them based on their individual risks, health history and preferences. If you have a mutation in the BRCA1 and BRCA2 genes (which accounts for about 5 percent to 10 percent of all breast cancers) or have already have found a lump in your breast, you are, of course, exempt from these recommendations.
Healthinfi.com raises some important points and has different recommendations. Here’s what it says.
- It’s tough to accurately identify the entire group of women who are at an average risk of breast cancer and that risk can be underestimated. For instance, risk is inherited equally from both parents not just the mother’s side yet some risk assessment models fail to recognize this.
- If a woman’s medical records are not updated, new cases of breast cancers or related cancers in her family may not be factored into the equation.
- The new ACS guidelines failed to take a newer, more accurate and sensitive screening method into consideration: 3D mammography (also known as tomosynthesis), which has resulted in significantly fewer false positives and increased detection of cancers. This type of improved screening also finds more serious invasive cancers that can metastasize, or spread.
- Women should take advantage of all three available tools, including high-quality mammography and clinical and self-exam of breasts to ensure the best chance of early detection.
- All women should have annual mammograms starting at age 40. Those at a higher risk of breast cancer should talk to their doctors about starting at a younger age and consider additional screening tools like MRI or ultrasound to maximize their opportunity for early detection.
What other organizations and top cancer centers are saying
Memorial Sloan Kettering says women at average risk should start mammograms at age 40.
So does MD Anderson, the American College of Radiology, the Society of Breast Imaging and the National Comprehensive Cancer Network.
In the end, the choice you make should be carefully weighed and discussed with your health care professional, who can guide you and help you reach an informed decision.
Discussing the benefits and harms, your personal beliefs, as well as your family history, can help reveal the best answer to that often-perplexing question: When should I get a mammogram?
Here are the new ACS guidelines for women at average risk:
- Ages 40 to 44: Annual mammograms are now optional.
- Ages 45 to 54: Women should start annual mammography at age 45.
- Ages 55 and older: Women can transition to having mammograms every other year, though they may choose to continue annual screening. One rationale was that cancers tend to grow slowly and are less aggressive in postmenopausal women.
- Older ages: Screening should continue as long as a woman is in good health, with a life expectancy of at least 10 years.
- Clinical breast exams done by health professionals are no longer recommended because of the “absence of clear evidence” that they add significantly to breast cancer detection beyond mammography; they also increase false-positives. While monthly self-exams are not advised either, women should be familiar with how their breasts normally look and feel and report changes to their health care providers right away, the ACS advises.

Pros and Cons of Mammograms
Before getting into the reasoning behind all of the various guidelines, let me remind all women of two vital points:
First, these are all just recommendations based on large population data, and are intended only for women who are at average risk of breast cancer.
Remember that every woman is different. Instead of relying on broad-based recommendations, you should base your decisions regarding the timing and frequency of mammograms on your family history, your personal risk factors, and conversations with your doctor.
Mammograms have proven to be extremely useful in detecting breast cancer, often in the early stages, giving women and their doctors more time and options for treatment.
So why would anyone suggest doing fewer of them?
The truth is that mammograms aren’t perfect, and they can lead to unnecessary treatments and unintended consequences. The National Cancer Institute estimates that half of all women who get annual mammograms over a 10-year period will experience a false positive — meaning they will be called back for additional imaging or a biopsy for what ends up being a non-cancerous lesion. About one out of every six of those women will undergo biopsies, but only 5 percent of women recalled for further testing are found to have cancer.
In other cases, breast cancers that are asymptomatic and pose no threat to a woman’s life are detected and treated. These cases are commonly overtreated, subjecting women to the pain, cost, and lasting effects of surgery, radiation, hormone therapy, or chemotherapy.
In some cases, treatments can cause women to develop lymphedema (irreversible swelling in the arms and legs), heart problems, or other types of cancer due to exposure to radiation — all because tumors were treated aggressively and unnecessarily.
As for the idea of getting mammograms every other year, it’s important to remember that, for the most part, breast cancers are slow-growing. Even if a woman develops a tumor in the 24 months between mammograms, there is often still time to treat it effectively.
How to Make Your Own Mammogram Decision
The guidelines also suggest doing away with clinical breast exams, and recommend that we stop teaching women how to do breast self-exams. That may seem extreme, but the truth is there is no proof that exams of any kind have ever consistently prevented deaths.
That’s not to say that you shouldn’t be aware of your body, of course. If you notice any changes in your breasts, such as dimpling, redness, soreness, puckering, or changes in size, by all means see your doctor.
The bottom line is that every woman is unique. Before ever scheduling your first mammogram, you should get to know your family history and understand your risks.
I wasn’t surprised to learn I had breast cancer, but it was a surprise to hear it at age 40, after a routine mammogram. My mother was a breast cancer survivor, and so was my grandmother. In that regard, I was not at an “average” woman for whom these guidelines are written.
I knew my risks, took my health into my own hands, and worked closely with my doctor every step of the way. And regardless of your take on the lastest changes to the mammogram guidelines, you should do the same.
For more information visit us our website: https://www.healthinfi.com
0 200Review
-
Very Nice Article....




No Comments