Overview
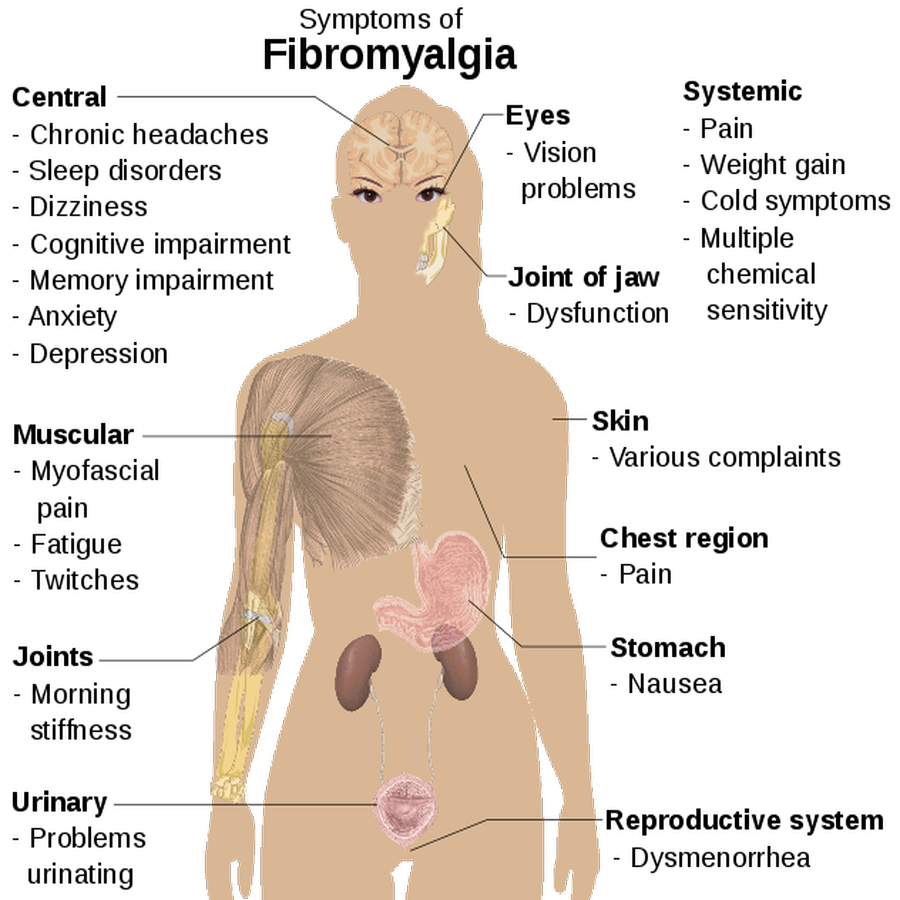
Fibromyalgia is a chronic disorder characterized by widespread pain and reduced pressure pain threshold (tender points). People with fibromyalgia may also experience fatigue, sleep disturbances, stiffness, deep tenderness, soreness and achiness, increased headaches or facial pain, difficulty concentrating, forgetfulness and problems multitasking. Patients with fibromyalgia frequently report functional impairment and diminished quality of life.
The cause of fibromyalgia is unknown, but recent evidence suggests it is associated with abnormalities in the central nervous system processing of pain. Fibromyalgia patients develop an increased response to painful stimuli and experience pain from non-painful stimuli such as touch. This is thought to reflect enhanced pain processing that is characteristic of central pain sensitization.
Patients with fibromyalgia have been found to have elevated levels of substance P in their spinal fluid, a chemical that helps transmit pain signals from the brain. Fibromyalgia patients also have been found to have reduced spinal fluid levels of neurotransmitters such as norepinephrine and serotohttp that are involved in the pain inhibitory pathways in the central nervous system. Scientists are investigating how the brain and spinal cord process pain and how substance P and other neurotransmitters fit into the process.
Recent studies have found that fibromyalgia runs in families, suggesting a genetic predisposition to the disorder.
Diagnosing fibromyalgia has been controversial because there are no specific laboratory tests to identify the disorder. Until recently, many health care professionals thought fibromyalgia was primarily caused by psychological factors. In recent years, however, health care professionals have come to understand that psychological factors do not necessarily cause fibromyalgia but rather may contribute to an increased risk for disability associated with fibromyalgia. Furthermore, depression andanxiety disorders may share some of the same chemical imbalances that are associated with fibromyalgia. For example, low levels of certain chemicals in the brain, including serotonin and norepinephrine, are linked not only to depression, but also to pain and fatigue.
It is estimated that at least 2 percent of the U.S. adult population has fibromyalgia. This condition occurs more commonly in women of childbearing age (as many as 80 to 90 percent of those diagnosed with fibromyalgia are women), but children, postmenopausal women, the elderly and men can also be affected. Because diagnosis can be difficult, it may take several years to correctly diagnose. Fortunately, with increased awareness of the disorder, many patients are getting diagnosed earlier than in the past, which may improve long-term outcomes. The severity of fibromyalgia symptoms varies. For some women, pain or other symptoms can be so intense that they interfere with daily activities. For others, symptoms may cause discomfort but are not incapacitating. However, fibromyalgia can be quite disabling. Many people with the condition report that it interferes with their lives at home and work and gets in the way of their personal relationships. Plus, dealing with a disorder that is so often misunderstood can be extremely frustrating.
Treating fibromyalgia requires a comprehensive approach, encompassing symptom management and lifestyle adaptation. It also requires a team approach with the patient and health care professionals, including physicians, physical therapists and cognitive therapists. Fibromyalgia is a disorder characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory and mood issues. Researchers believe that fibromyalgia amplifies painful sensations by affecting the way your brain processes pain signals.
Symptoms sometimes begin after a physical trauma, surgery, infection or significant psychological stress. In other cases, symptoms gradually accumulate over time with no single triggering event. Women are more likely to develop fibromyalgia than are men. Many people who have fibromyalgia also have tension headaches, temporomandibular joint (TMJ) disorders, irritable bowel syndrome, anxiety and depression.
While there is no cure for fibromyalgia, a variety of medications can help control symptoms. Exercise, relaxation and stress-reduction measures also may help.
Diagnosis
Fibromyalgia is defined by the American College of Rheumatology as chronic (three months or more) widespread pain and pain on palpation of 11 of 18 tender points. Common associated symptoms include sleep problems, fatigue, cognitive impairment and mood disturbances. Even though it is recognized as a legitimate clinical entity, experts think it continues to be underdiagnosed or misdiagnosed.
If you suspect you may have this condition, discuss your symptoms with your primary care physician. Your primary physician may refer you to other medical professionals for further evaluation. For example, you may be referred to a rheumatologist, who specializes in disorders affecting the joints, muscles, tendons, ligaments and bones.
Even with the right doctor, fibromyalgia can be difficult to diagnose. Many of its symptoms are variable, so they’re not always there, and many are common across numerous medical conditions. There is no specific medical test for fibromyalgia. The American College of Rheumatology criteria for fibromyalgia require that a person has had widespread pain above and below the waist, on both sides of the body and in the axial skeleton, for at least three months, as well as pain on palpation of at least 11 of 18 specific tender point sites. You can view an illustration of common tender points in fibromyalgia at www.healthinfi.com.
These criteria were designed to standardize classification for participants in clinical trials, and some health care providers find them difficult to understand and use. The American College of Rheumatology has also developed preliminary diagnostic criteria for diagnosing fibromyalgia that do not require tender point exams. Instead, these criteria involve using combined numerical scores that reflect severity of pain and other symptoms. These criteria may include a combination of chronic, widespread pain and other commonly associated symptoms such as fatigue and sleep disturbance.
Your health care provider will diagnose you based on your symptoms, a complete medical history, physical exam and tests to rule out other conditions such as lupus, rheumatoid arthritis or hypothyroidism. In addition to the pain, sleep problems and fatigue are common in patients with fibromyalgia. Other associated symptoms may include the following:
- Cognitive disorders, most often short-term memory lapses and difficulty concentrating
- Unusual sensitivity to cold, especially in the hands and feet, often accompanied by color changes, numbness and tingling; this condition is known as Raynaud’s phenomenon (also called Raynaud’s syndrome)
- Urinary complaints, including a strong urge to urinate, frequent urination and pain in the bladder
- Painful menstrual periods
- Heightened sensitivity to noises, bright lights, odors and touch
- Painful sexual intercourse
- Stiffness, particularly in the early morning, after prolonged sitting or standing, or with changes in temperature or relative humidity
- Light-headedness and/or balance problems.
- Abdominal discomfort
- Paresthesia (numbness or tingling), often in the hands or feet
Fibromyalgia also may coexist with other chronic painful conditions such as osteoarthritis, rheumatoid arthritis or low back pain. It frequently is accompanied by central sensitivity syndromes, including irritable bowel syndrome, interstitial cystitis, restless leg syndrome, temporomandibular disorder (TMD), tension-type headaches or migraines, chronic pelvic pain, endometriosis and chronic prostatitis. There also appears to be a link between fibromyalgia and chronic fatigue syndrome (CFS). Up to 70 percent of people with fibromyalgia fit the criteria for CFS.
Fibromyalgia can affect mood and cause psychological distress, and research has shown that a lifetime history of mood or anxiety disorders is common in people with fibromyalgia. When depression or anxiety is present, treatment is important because they can make fibromyalgia symptoms worse and can interfere with successful management. Even if you don’t have depression, antidepressants may be prescribed for pain relief and to help you sleep.
Recent studies suggest that depression and fibromyalgia may share a biological link. Low levels of certain chemicals in the brain, including serotonin and norepinephrine, are associated not only with depression, but also with pain and fatigue. Still, not everyone with fibromyalgia will experience depression or anxiety. Up to 74 percent of people with fibromyalgia experience depression and an estimated 60 percent experience anxiety at some point in their lives.
In the past, doctors would check 18 specific points on a person’s body to see how many of them were painful when pressed firmly. Newer guidelines don’t require a tender point exam. Instead, a fibromyalgia diagnosis can be made if a person has had widespread pain for more than three months — with no underlying medical condition that could cause the pain.

Blood tests
While there is no lab test to confirm a diagnosis of fibromyalgia, your doctor may want to rule out other conditions that may have similar symptoms. Blood tests may include:
- Complete blood count
- Erythrocyte sedimentation rate
- Cyclic citrullinated peptide test
- Rheumatoid factor
- Thyroid function tests
Treatment
Treating fibromyalgia requires a comprehensive, multidisciplinary approach. Among the most effective treatments are medications, exercise, sleep management and cognitive behavioral therapy. Treatment centers on managing the symptoms of fibromyalgia; there is no cure. Since symptoms vary, so does treatment.
In general, treatments for fibromyalgia include both medication and self-care. The emphasis is on minimizing symptoms and improving general health. No one treatment works for all symptoms.
Therapy
A variety of different therapies can help reduce the effect that fibromyalgia has on your body and your life. Examples include:
- Physical therapy. A physical therapist can teach you exercises that will improve your strength, flexibility and stamina. Water-based exercises might be particularly helpful.
- Occupational therapy. An occupational therapist can help you make adjustments to your work area or the way you perform certain tasks that will cause less stress on your body.
- Counseling. Talking with a counselor can help strengthen your belief in your abilities and teach you strategies for dealing with stressful situations.
Alternative medicine
Complementary and alternative therapies for pain and stress management aren’t new. Some, such as meditation and yoga, have been practiced for thousands of years. But their use has become more popular in recent years, especially with people who have chronic illnesses, such as fibromyalgia.
Several of these treatments do appear to safely relieve stress and reduce pain, and some are gaining acceptance in mainstream medicine. But many practices remain unproved because they haven’t been adequately studied.
- Acupuncture. Acupuncture is a Chinese medical system based on restoring normal balance of life forces by inserting very fine needles through the skin to various depths. According to Western theories of acupuncture, the needles cause changes in blood flow and levels of neurotransmitters in the brain and spinal cord. Some studies indicate that acupuncture helps relieve fibromyalgia symptoms, while others show no benefit.
- Massage therapy. This is one of the oldest methods of health care still in practice. It involves use of different manipulative techniques to move your body’s muscles and soft tissues. Massage can reduce your heart rate, relax your muscles, improve range of motion in your joints and increase production of your body’s natural painkillers. It often helps relieve stress and anxiety.
- Yoga and tai chi. These practices combine meditation, slow movements, deep breathing and relaxation. Both have been found to be helpful in controlling fibromyalgia symptoms.
Exercise
Exercise may seem an impossibly tall order—after all, if you’re in pain, how can you work out? But if you don’t get regular aerobic exercise, your muscles become weaker, making them even more susceptible to pain during everyday tasks. In fact, studies find that aerobic exercise such as swimming and walking improves muscle fitness and reduces muscle pain and tenderness in people with fibromyalgia. Stick with a low-impact exercise program such as walking, swimming or water aerobics, and be sure to discuss any new exercise program with your health care professional if you’ve been inactive.
Exercise can also help you sleep better, improve your mood, reduce pain, increase flexibility, improve blood flow, help you manage your weight and promote general physical fitness. It is inexpensive and, if done correctly, has few negative side effects. When you exercise, listen to your body and know when to stop or slow down to prevent pain caused by over-exercising. Talk to your health care professional about how to introduce exercise into your life in a way that is tolerable and safe. In some situations, your health care professional may recommend physical therapy with therapists knowledgeable in fibromyalgia management, who can help you with a physical rehabilitation program.
Attitude Can Improve Symptoms
Your psychological outlook is important, with studies finding benefits from cognitive therapy for women with fibromyalgia. Specifically, studies find, negative thinking increases stress and affects your perception of pain, so learning to minimize and control these thoughts can improve your symptoms.
The key is not so much to “think positively,” but to “think non-negatively.” So when negative thoughts occur, ask yourself: “Does this thought benefit me in any way—does it improve the way I feel, advance my goals or improve a relationship?”
Strategies for dealing with negative thoughts include:
- Alternative interpretation. You might start with a fairly neutral thought such as “I’m tired today.” From there, it’s easy to go negative—”I feel lousy. I won’t get anything done today.” An alternative, non-negative interpretation could be: “What strategies can I try to sleep better so I won’t feel so tired?”
- Anti-catastrophic reappraisal. This technique consists of challenging negative thoughts. You might have a catastrophic thought such as, “This fatigue is never going to get better. I’ll never wake up with any energy.” When you have such thoughts, ask yourself: How likely is it really that the fatigue will never get better? Have you ever been more fatigued than you are today?
- Coping statements. In these statements, you tell yourself that you can handle these symptoms, and remind yourself of strategies you’ve used in the past to cope with or alleviate symptoms.
- Label shifting. How we describe things influences our overall mood and physical sense of well-being. So instead of viewing your pain as excruciating, try describing it as uncomfortable, or view it as a warning that maybe you’ve been overdoing it.
Symptoms
Symptoms of fibromyalgia include:
- Widespread pain. The pain associated with fibromyalgia often is described as a constant dull ache that has lasted for at least three months. To be considered widespread, the pain must occur on both sides of your body and above and below your waist.
- Fatigue. People with fibromyalgia often awaken tired, even though they report sleeping for long periods of time. Sleep is often disrupted by pain, and many patients with fibromyalgia have other sleep disorders, such as restless legs syndrome and sleep apnea.
- Cognitive difficulties. A symptom commonly referred to as “fibro fog” impairs the ability to focus, pay attention and concentrate on mental tasks.
- Irritable bowel syndrome
- Migraine and other types of headaches
- Interstitial cystitis or painful bladder syndrome
- Temporomandibular joint disorders
Common Symptoms and Related Conditions
Many people with fibro — also called fibromyalgia syndrome or FMS — may have:
- Pain and tender points
- Fatigue
- Sleep problems
- Concentration and memory problems, known as “fibro fog”
- Anxiety or depression
- Morning stiffness
- Numbness, and tingling in hands, arms, feet, and legs
- Headaches
- Irritable bowel syndrome
- Problems with peeing
- Painful menstrual cramps
Pain and Tender Points
Almost all people with fibromyalgia ache all over. It can feel similar to osteoarthritis, bursitis, and tendinitis, but it’s over your entire body. This is usually what makes you go see your doctor.
The pain can be deep, sharp, dull, throbbing, or aching. You feel it in your muscles, tendons, and ligaments around the joints. For some people, the pain comes and goes. It could travel throughout your body. You may also have tender points — specific spots around your joints that hurt when you press them with a finger. If you press a tender point on a person without fibromyalgia, they’ll just feel pressure. But that same pressure would be very painful for someone with fibro. These tender points are in predictable places on the body. They’re often under the surface of the skin, not in areas of deep pain. It’s the tissue around the muscles and joints that hurts rather than the joints themselves.
Sleep Problems
The majority of people with fibromyalgia have trouble sleeping. You may be able to fall asleep, but your sleep is light and easily disturbed. When you get up in the morning, you’re exhausted and not refreshed. It doesn’t help the fatigue.
Tests done in sleep labs show that people with fibro are constantly interrupted by bursts of brain activity similar to what happens in the brain when they’re awake. These interruptions limit how much time you spend in deep sleep, when your body restores itself, and you feel run down as a result.
Mood Disorders
Up to half of all people with fibromyalgia have depressionor an anxiety disorder when they’re diagnosed with fibro.
Dealing with being fatigued and in pain all the time can be stressful. You probably worry about keeping up with life and what you can do to feel better. You may become less active and more withdrawn, which can lead to depression.
It’s also possible that anxiety and depression may actually be a part of fibromyalgia, like the pain.
People diagnosed with fibromyalgia and depression have a hard time with concentration and short-term memory, which make it hard to remember day-to-day things, like where they’ve put their keys or plans they’ve made for lunch tomorrow.
Morning Stiffness
Most people with fibromyalgia feel like they need to “loosen up” after getting out of bed before they can start their day. The muscles and joints of their back, arms, and legs feel stiff. It’s not typical creakiness. It’s more like the stiffness someone with rheumatoid arthritis feels.
Although some people say it lasts only a few minutes, the stiffness usually sticks around for more than 15 to 20 minutes each day. Sometimes it lasts for hours, and it could linger all day.
While the cause of numbness, tingling, and burning is unclear, many people with fibro feel them. These sensations, called paresthesia, tend to happen randomly. They may last a few minutes, or they may be constant.
The feelings can be especially bothersome in the mornings along with morning stiffness. But they generally don’t get in the way of doing things.
Headaches
Up to 2 out of 5 people with fibro also get migraine or tension headaches regularly. They may be a result of pain in your neck and upper back. They’re often caused by tight neck muscles. They may also be caused by tender points over the back of your head and neck.
Headaches can make it much harder for you to live with fibro and manage the disease.
Irritable Bowel Syndrome
About two-thirds of people with fibromyalgia often have belly pain, gas, and bloating and feel like throwing up. They can also have constipation and diarrhea.
Many have acid reflux or gastroesophageal reflux disease (GERD), too.
Feeling the urge to go a lot, hurting when you do, or a leaky bladder can happen when you have fibromyalgia.
These symptoms could also be caused by bladder and kidney diseases, such as an infection.
Menstrual Cramps
Women with fibromyalgia may have unusually painful menstrual cramps, often for years, along with their other symptoms.
Restless Legs Syndrome
This usually affects your feet and legs below your knees. It may hurt, but more often it feels like you need to move your legs to try to make them comfortable. It’s especially bothersome at night because it can keep you from sleeping.
A lingering tiredness and feeling drained is another big complaint. People often feel tired even when they should feel rested, such as after a good night’s sleep. Some say it’s like having the flu. Some compare it to working long hours and missing a lot of sleep.
You may feel too tired to exercise or more tired after a workout. Simple things such as grocery shopping or cooking dinner could wipe you out. Starting a project such as folding clothes or ironing could seem like too much effort. You might even be too tired for sex.
Causes
Doctors don’t know what causes fibromyalgia, but it most likely involves a variety of factors working together. These may include:
- Genetics. Because fibromyalgia tends to run in families, there may be certain genetic mutations that may make you more susceptible to developing the disorder.
- Infections. Some illnesses appear to trigger or aggravate fibromyalgia.
- Physical or emotional trauma. Fibromyalgia can sometimes be triggered by a physical trauma, such as a car accident. Psychological stress may also trigger the condition.
Risk factors
Risk factors for fibromyalgia include:
- Your sex. Fibromyalgia is diagnosed more often in women than in men.
- Family history. You may be more likely to develop fibromyalgia if a relative also has the condition.
- Other disorders. If you have osteoarthritis, rheumatoid arthritis or lupus, you may be more likely to develop fibromyalgia.
Medications
Pregabalin (Lyrica), previously approved by the U.S. Food and Drug Administration for adjunctive treatment of partial onset seizures and certain types of neuropathic pain, was the first medication to be approved for treating fibromyalgia. Common side effects may include dizziness, sleepiness, dry mouth, swelling, blurred vision, weight gain and difficulty with concentration and attention.
Duloxetine (Cymbalta), previously approved for the treatment of major depression, generalized anxiety disorder and diabetic peripheral neuropathic pain, is also approved for treating fibromyalgia and for treatment of chronic musculoskeletal pain due to chronic osteoarthritis pain and chronic low back pain. Common side effects of duloxetine may include nausea, dry mouth, constipation, sleepiness, increased sweating and decreased appetite. And the third medication approved for the treatment of fibromyalgia is milnacipran (Savella). Common side effects of milnacipran may include nausea, constipation, hot flush, increased sweating, vomiting, palpitations, increased heart rate, dry mouth and hypertension.
Other medications that have medical evidence to support their use in fibromyalgia but are not currently indicated for the treatment of fibromyalgia include the following:
- Antidepressants, including the tricyclic antidepressant amitriptyline (Elavil) and the selective serotonin reuptake inhibitor fluoxetine (Prozac).
- Tramadol (Ultram), a centrally acting analgesic for pain relief, which may be taken with or without acetaminophen.
- Muscle relaxant, cyclobenzaprine (Flexeril), to improve sleep and reduce pain and muscle spasms.
- Anticonvulsant, gabapentin (Neurontin), which is similar to pregabalin (Lyrica).
Complementary Approaches
In addition to medication, a variety of alternative and lifestyle approaches can help you deal with symptoms of pain. However, be aware that there is limited scientific evidence to support these approaches at this time.
- Massage therapy can be very effective short-term. For the best results, look for a licensed massage therapist who has worked with fibromyalgia patients before.
- Moist heat supplied by warm towels, hot packs, a hot bath or a shower can be used at home for 15 to 20 minutes three times a day to relieve symptoms.
- Cold supplied by a bag of ice or frozen vegetables wrapped in a towel helps reduce pain when used for 10 to 15 minutes at a time. Don’t do this, however, if you have Raynaud’s phenomenon.
- Hydrotherapy (water therapy) can reduce pain during exercise and help you improve endurance and conditioning. Exercising in a large pool may be easier because water has a buoying effect. Community centers, YMCAs and YWCAs have water exercise classes developed for people with arthritis and other conditions that may make exercise painful. To find a YMCA or YWCA in your area, check. Some patients also find relief from the heat and movement provided by a whirlpool.
- Relaxation techniques help reduce pain and anxiety. These include meditation and guided imagery. Check with local recreation centers and hospitals for courses.
- Acupuncture is an ancient Chinese treatment that is often used for pain relief. A qualified acupuncturist places very thin needles in certain parts of your body. Some researchers believe that the needles may stimulate deep sensory nerves that tell the brain to release natural painkillers (endorphins). However, the well-controlled studies examining acupuncture as a treatment for fibromyalgia symptoms did not find acupuncture to be more effective than a placebo treatment for fibromyalgia, so it is difficult to know for sure if the practice produces any specific benefits. Acupressure is similar to acupuncture, but pressure is applied to the sites instead of needles.
- Biofeedback is a form of therapy used to train your mind to understand and, to a degree, control your own physiological responses. An electronic device provides information about a body function (such as heart rate) so you learn to consciously control that function. For instance, it can help you learn to relax your muscles.
Prevention
There is no known way to prevent fibromyalgia. Instead, the most important thing is to find a way to manage it and to find a health care team to help you.
Once diagnosed, you should monitor your pain, noting activities that increase it and therapeutic approaches that reduce it. Repetitive activities may temporarily make things worse, such as sitting in one position for a long time. Pain can also flare when doing chores like cleaning, typing or driving for hours with your arms in the same tensed position. Even reading in a slumped position may trigger pain.
The key is to make adjustments—change positions, take a quick break or give your back, arms or neck more supportbefore the pain worsens. You can also make adjustments to your cleaning routine, using lighter appliances to minimize muscular distress. Obviously, fibromyalgia can interfere with work, especially if your job involves a repetitive physical task, heavy lifting or working outdoors when it’s cold. Research finds that fibromyalgia patients tend to do better if they work, however, so if the disease is affecting your ability to work, talk to your health care professional about how you can reduce the strain. Most important is to improve your physical conditioning and endurance, find ways to manage and reduce stress and maintain a regular schedule.
Facts to Know
- Fibromyalgia is a chronic disorder characterized by widespread musculoskeletal pain and multiple tender points. “Tender points” refers to tenderness that occurs in localized areas, particularly in the neck, spine, shoulders and hips.
- People with fibromyalgia may also experience fatigue, sleep disturbances, morning stiffness, irritable bowel syndrome, anxiety, depression and other symptoms.
- At least 2 percent of the U.S. adult population suffers from fibromyalgia, and it predominantly affects women. The condition primarily occurs in women in early and middle adulthood, but children, the elderly and men can be affected.
- There is no cure for fibromyalgia, though the disorder can be successfully managed.
- Fibromyalgia is defined based on widespread pain in combination with tenderness in at least 11 of 18 specific tender point sites for at least three months. There are no lab tests to confirm a diagnosis, although some tests may be used to rule out other conditions with similar symptoms, such as rheumatoid arthritis or lupus.
- There appears to be a link between fibromyalgia and chronic fatigue syndrome (CFS). Up to 70 percent of people with fibromyalgia fit the criteria for CFS.
- Low-impact aerobic exercise such as walking and swimming can help manage the symptoms of fibromyalgia. Physical therapy and stretching exercises also help.
- A variety of medications are used to treat fibromyalgia, including the three FDA-approved medications for fibromyalgia: pregabalin (Lyrica), duloxetine (Cymbalta) and milnacipran (Savella). Additional medications include other antidepressants and anti-seizure drugs.
- If you are diagnosed with fibromyalgia, you should monitor your pain, noting activities that increase it and therapeutic approaches that improve it. Repetitive activities may temporarily exacerbate the condition, as may sitting in one position for a long time.
- Studies find that negative thinking increases stress and affects your perception of pain, so learning to minimize and control these thoughts can improve your symptoms. The key is not so much to “think positively,” but to “think non-negatively.
Key Q&A
- What are the symptoms of fibromyalgia?The classic symptoms of fibromyalgia are widespread pain, tenderness, fatigue and problems sleeping. Other symptoms include (but are not limited to) cognitive dysfunction, stiffness, irritable bowel syndrome, depression and anxiety.
- What causes the disease?No one knows exactly what causes fibromyalgia, but current thinking centers on a theory called “central sensitization,” which means that people with fibromyalgia have increased sensitivity to pain signals in their brains, resulting in a lower threshold for pain. Women make up 80 to 90 percent of people with fibromyalgia. The most common time for women to develop the condition is in early and middle adulthood.
- I think I may have fibromyalgia, but my doctor doesn’t know much about the disease. What should I do?Ask for a referral to a rheumatologist or physiatrist who is knowledgeable about the disease. A rheumatologist is a doctor who specializes in disorders that affect the joints, muscles, tendons, ligaments and bones. A physiatrist specializes in diagnosing and treating injuries and diseases causing pain, loss of function and disability.
- I have heard that aerobic exercise is good for fibromyalgia, but how can I possibly exercise when I’m in such pain?If you’ve been sedentary for a while, you should start out with stretching exercises for several weeks. Therapy in warm water is easier than therapy on land. Heat, massage, hydrotherapy (exercising in a pool or using a whirlpool) and relaxation therapy are among the strategies that may help. Discuss any exercise plan with a health care professional before you start. A physical therapist knowledgeable in fibromyalgia may also help you develop a physical activity program.
- What medications are available to treat fibromyalgia pain?The U.S. Food and Drug Administration has approved three drugs for the treatment of fibromyalgia symptoms: pregabalin (Lyrica), duloxetine (Cymbalta) and milnacipran (Savella). Other medications commonly used include other antidepressants and anti-seizure drugs.
- What medications are available to treat the sleeping problems associated with fibromyalgia?Some sedating antidepressants are sometimes effective, and occasionally a doctor may prescribe a short-term course of sleeping pills. A muscle relaxant called cyclobenzaprine (Flexeril) may temporarily help to improve sleep and reduce pain. Pregabalin (Lyrica) and gabapentin (Neurontin) have been shown to improve sleep in patients with fibromyalgia. If you’re having trouble sleeping, you may also want to employ standard nonmedical remedies and good sleep hygiene, such as avoiding caffeine, forgoing naps, avoiding alcohol and going to bed at the same time every night. A sleep specialist may help to identify and treat other sleep disorders such as sleep apnea that can occur in some patients with fibromyalgia.
- What is the relationship between fibromyalgia and depression?It is estimated that up to 74 percent of those with fibromyalgia experience depression and about 60 percent experience anxiety at some point in their lives. What causes the correlation between fibromyalgia and depression is unclear, but it may be related to low levels of certain brain chemicals, including serotonin and norepinephrine.
- Why has the diagnosis of fibromyalgia been so controversial?Because up until the late 1990s, no pathological origin for the chronic, persistent pain could be found. Now multiple studies link the condition to abnormal pain processing in the central nervous system. Because women who presented with the syndrome often had depression and anxiety along with their condition, some doctors thought fibromyalgia was primarily caused by psychological factors. In recent years, skepticism has largely given way to interest in more fully characterizing symptoms and finding effective treatments.
- What are some nonmedical approaches to treating the disease?Medications may be necessary, but there are a number of day-to-day strategies for coping with the disease. A fibromyalgia support group can help provide insight, advice and support. You can improve sleep by avoiding naps and caffeine and by going to bed at a consistent time. You should also monitor your pain and adjust your activities accordingly. To manage pain, you can try massage, heat and cold packs, relaxation therapy, water therapy (such as whirlpools), biofeedback and acupuncture or acupressure.
For more information visit us our website: https://www.healthinfi.com
0 200
Review
-
I like This Post,"good for your work"



No Comments